Med 1-200 .

Cardiovascular Mastery Quiz
Test your knowledge and understanding of cardiovascular health with our comprehensive quiz designed for medical professionals, students, and enthusiasts alike. Featuring 200 challenging questions, this quiz will help you assess your expertise in diagnosing and managing heart-related conditions.
Key Features:
- 200 questions covering a range of cardiovascular topics.
- Multiple-choice format to test critical thinking and decision-making skills.
- Ideal for studying for exams or enhancing your medical knowledge.
1. A 60-year-old male patient is receiving aspirin, an angiotensin-converting enzyme inhibitor, nitrates, and a beta-blocker for chronic stable angina. He presents to the ER with an episode of more severe and long-lasting angina chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. Which of the following is the best course of action?
A. Admit the patient and add intravenous digoxin.
B. Admit the patient and begin low-molecular-weight heparin.
C. Admit the patient for thrombolytic therapy.
D. Admit the patient for observation with no change in medication.
E. Increase the doses of current medications and follow closely as an outpatient.
2. If the QRS complex is positive in leads II and aVF and negative in lead III, the mean electrical axis (MEA) is between:
A. -30° and 0°
B. 0° and +30°
C. +30° and +60°
D. +60° and +90°
E. +90° and +120
3. While palpating the pulse of a patient, you note that the pulse wave has two peaks. You auscultate the heart and are certain that there is only one heartbeat for each two pulse waves. Which of the followi ng best describes this finding?
A. Pulsus alternans
B. Dicrotic pulse
C. Pulsus parvus et tardus
D. Pulsus bigeminus
E. Pulsus bisferien
4. A 75-year-old patient presents to the ER after a syncopal episode. He is again alert and in retrospect describes occasional substernal chest pressure and shortness of breath on exertion. His blood pressure is 110/80 and lungs have a few bibasilar rales. Which auscultatory finding would best explain his findings?
A. A harsh systolic crescendo-decrescendo murmur heard best at the upper right sternal border
B. A diastolic decrescendo murmur heard at the mid-left sternal border
C. A holosystolic murmur heard best at the apex
D. A midsystolic click
E. A pericardial rub
5. A 72-year-old male comes to the office with intermittent symptoms of dyspnea on exertion, palpitations, and cough occasionally productive of blood. On cardiac auscultation, a low-pitched diastolic rumbling murmur is faintly heard at the apex. What is the most likely cause of the murmur?
A. Rheumatic fever as a youth
B. Long-standing hypertension
C. A silent MI within the past year
D. A congenital anomaly
E. Anemia from chronic blood loss
6. You are helping with school sports physicals and see a 16-year-old boy who has had trouble keeping up with his peers. Which of the following auscultatory findings suggests a previously undiagnosed ventricular septal defect?
A. A systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise.
B. A systolic murmur at the pulmonic area and a diastolic rumble along the left sternal border.
C. A holosystolic murmur at the mid-left sternal border.
D. A diastolic decrescendo murmur at the mid-left sternal border.
E. A continuous murmur through systole and diastole at the upper left sternal border
7. A 42-year-old female with acute pericarditis develops jugular venous distention and hypotension. The ECG shows electrical alternants. Which of the following is the most likely additional physical finding? a. Basilar rales halfway up both posterior lung fields
A. Basilar rales halfway up both posterior lung fields
B. S3 gallop
C. Pulsus paradoxus
D. Strong apical beat
E. Epigastric tenderness
8. Which of the following patients has the lowest clinical probability for the diagnosis of pulmonary embolism (PE)?
A. A 21-year-old woman 2 days after a caesarean delivery.
B. A 55-year-old woman on estrogen replacement therapy who underwent a total hip replacement procedure 3 days ago.
C. A 39-year-old man who smokes cigarettes occasionally and underwent an uncomplicated appendectomy 2 months ago.
D. A 62-year-old man with pancreatic cancer.
E. A 45-year-old man with factor V Leiden deficiency.
9. A 29-year-old man is brought to the ED by EMS for a syncopal episode that occurred during a basketball game. A friend states that the patient just dropped to the ground shortly after scoring a basket on a fast break. On examination, you note a prominent systolic ejection murmur along the left sternal border and at the apex. An ECG reveals left ventricular hypertrophy, left atrial enlargement, and septal Q waves. You suspect the diagnosis and ask the patient to perform the Valsalva maneuver while you auscultate his heart. Which of the following is most likely to occur to the intensity of the murmur with this maneuver?
A. Decrease.
B. Increase.
C. Remain unchanged.
D. Disappear.
E. The intensity stays the same, but the heart skips a beat.
10. A 41-year-old intravenous drug abuser presents with shortness of breath and pleuritic chest pain. He is febrile with a temperature of 103.5°F. He has no skin lesions and funduscopic exam is negative. He has jugular venous distension that increases with compression of the liver. The liver is pulsatile. The jugular venous pulse shows a prominent v wave. The patient has splenomegaly. Heart auscultation reveals a holosystolic murmur heard best at the left lower sternal border. The murmur increases with inspiration (Müller maneuver). Which of the following is the most likely diagnosis?
A. Bacterial endocarditis
B. Pericarditis
C. Rheumatic fever
D. Mitral valve prolapse
E. Pericardial effusion
11. A 54-year-old man with a 20-year history of chronic obstructive lung disease has a heave that is palpable at the lower left sternal border at the third, fourth, and fifth intercostal spaces. Which of the following best explains the etiology of the heave?
A. It is probably a displaced point of maximum impulse (PMI)
B. It means the patient has congestive heart failure
C. It means that the patient has aortic stenosis
D. It means the patient has right ventricular hypertrophy
E. It means the patient has a pericardial effusion
12. Yesterday you admitted a 55-year-old white male to the hospital for an episode of chest pain, and you are seeking to rule out MI plus assess for any underlying coronary artery disease. The patient tends to be anxious about his health. On admission, his lungs were clear, but his heart revealed a grade 1/6 early systolic murmur at the upper left sternal border without radiation. Blood pressure readings have consistently been in the 140/90 to 150/100 range. Cardiac enzymes are normal. A resting ECG shows only left ventricular hypertrophy with secondary ST-T changes (“LVH with strain”). Why would a treadmill ECG stress test not be an appropriate test in this patient?
A. Anticipated difficulty with the patient’s anxiety (ie, he might falsely claim chest pain during the test)
B. Increased risk associated with high blood pressure readings
C. Concern about the heart murmur, a relative contraindication to stress testing
D. The presence of LVH with ST-T changes on baseline ECG
E. Concern that this represents the onset of unstable angina with unacceptable risk of MI with stress testing
13. A 67-year-old male presents to your office after community ultrasound screening revealed an aortic aneurysm measuring 3.0 x 3.5 cm. Physical examination confirms a palpable, pulsatile, nontender abdominal mass just above the umbilicus. The patient’s medical conditions include hypertension, hyperlipidemia, and tobacco use. What is the best recommendation for the patient to consider?
A. Watchful waiting is the best course until the first onset of abdominal pain.
B. Surgery is indicated except for the excess operative risk represented by the patient’s risk factors.
C. Serial follow- up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being aneurysmal size greater than 5 to 6 cm.
D. Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determina nt for surgery being involvement of a renal artery.
E. Unlike stents in coronary artery disease, endovascular stent grafts have proven unsuccessful in the management of AAAs

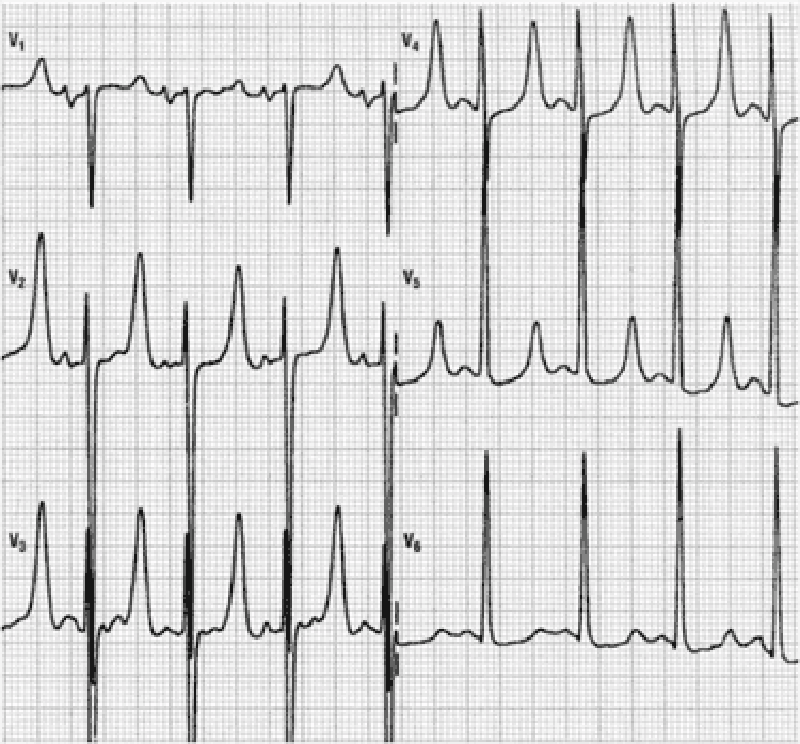
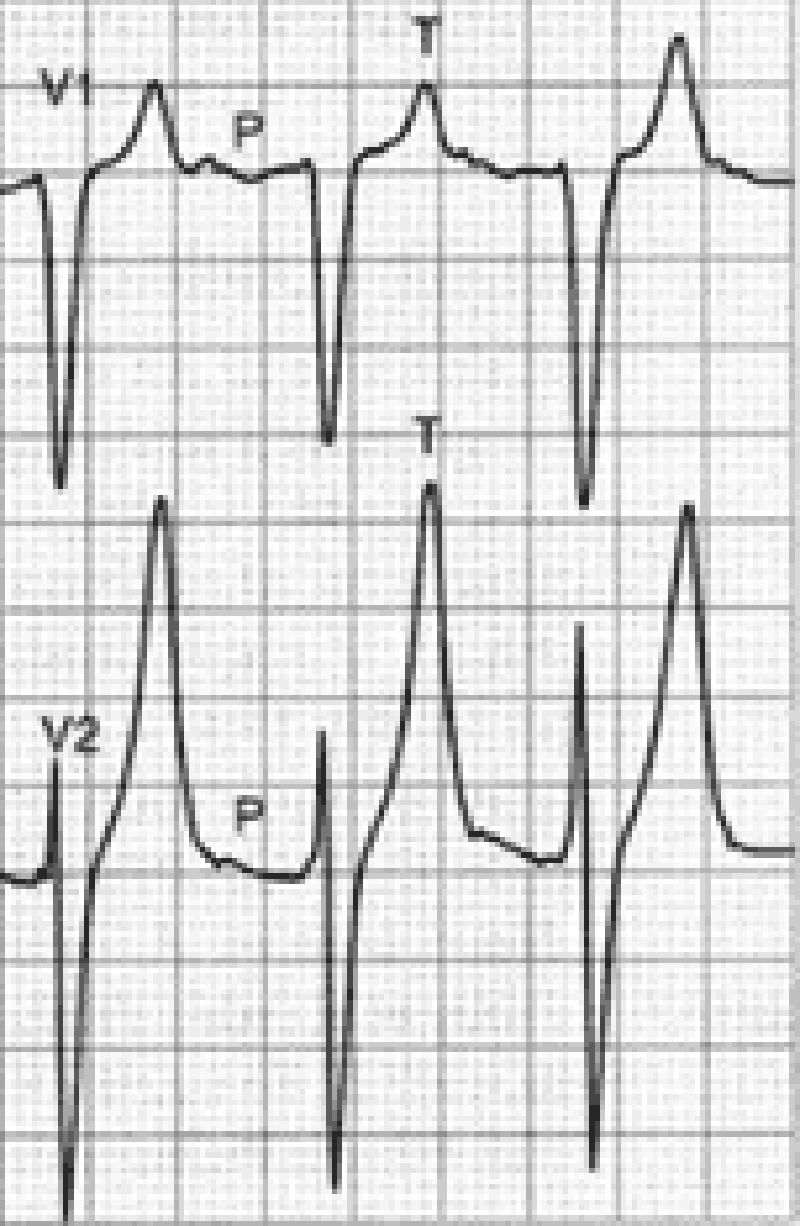
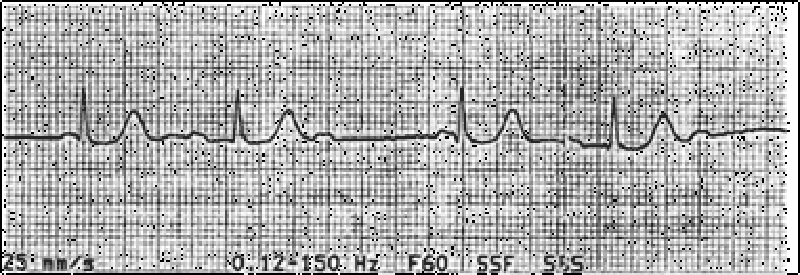
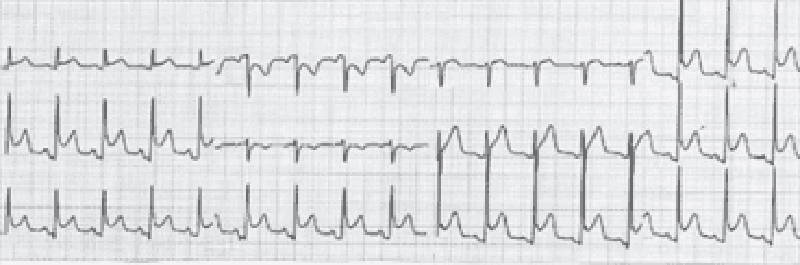
14. An 18-year-old male complains of fever and transient pain in both knees and elbows. The right knee was red and swollen for 1 day during the week prior to presentation. On physical examination, the patient has a low-grade fever. He has a III/VI, high pitched, apical systolic murmur with radiation to the axilla, as well as a soft, mid-diastolic murmur heard at the base. A tender nodule is palpated over an extensor tendon of the hand. There are pink erythematous lesions over the abdomen, some with central clearing. The following laboratory values are obtained: Hct: 42 WBC: 12,000/µL with 80% polymorphonuclear leukocytes, 20% lymphocytes ESR: 60 mm/h The patient’s ECG is shown below. Which of the following tests is most critical to diagnosis?
A. Blood cultures
B. Antistreptolysin O antibody
C. Echocardiogram
D. Antinuclear antibodies
E. Creatine kinase
15. A 50-year-old construction worker continues to have elevated blood ressure of 160/95 even after a third agent is added to his antihypertensive regimen. Physical examination is normal, electrolytes are normal, and the patient is taking no over-the-counter medications. Which of the following is the best next step for this patient?
A. Check pill count.
B. Evaluate for Cushing syndrome.
C. Check chest x-ray for coarctation of the aorta.
D. Obtain a renal angiogram.
E. Obtain an adrenal CT scan
16. A 35-year-old male complains of substernal chest pain aggravated by inspiration and relieved by sitting up. Lung fields are clear to auscultation, and heart sounds are somewhat distant. Chest x-ray shows an enlarged cardiac silhouette. Which of the following is the best next step in evaluation?
A. Right lateral decubitus chest x-ray
B. Cardiac catheterization
C. Echocardiogram
D. Serial ECGs
E. Thallium stress test
17. A 32-year-old male presents to your office with concern about progressive fatigue and lower extremity edema. He has experienced decreased exercise tolerance over the past few months, and occasionally awakens coughing at night. Past medical history is significant for sickle cell anemia and diabetes mellitus. He has had multiple admissio ns to the hospital secondary to vasoocclusive crises since the age of three. Physical examination reveals a displaced PMI, but is otherwise unremarkable. ECG shows a first degree AV block and low voltage. Chest x-ray shows an enlarged cardiac silhouette with clear lung fields. Which of the following would be the best initial diagnostic approach?
A. Order serum iron, iron-binding capacity, and ferritin level.
B. Order brain-natriuretic peptide (BNP)
C. Order CT scan of the chest.
D. Arrange for placement of a 24-hour ambulatory cardiac monitor.
E. Arrange for cardiac catheterization.
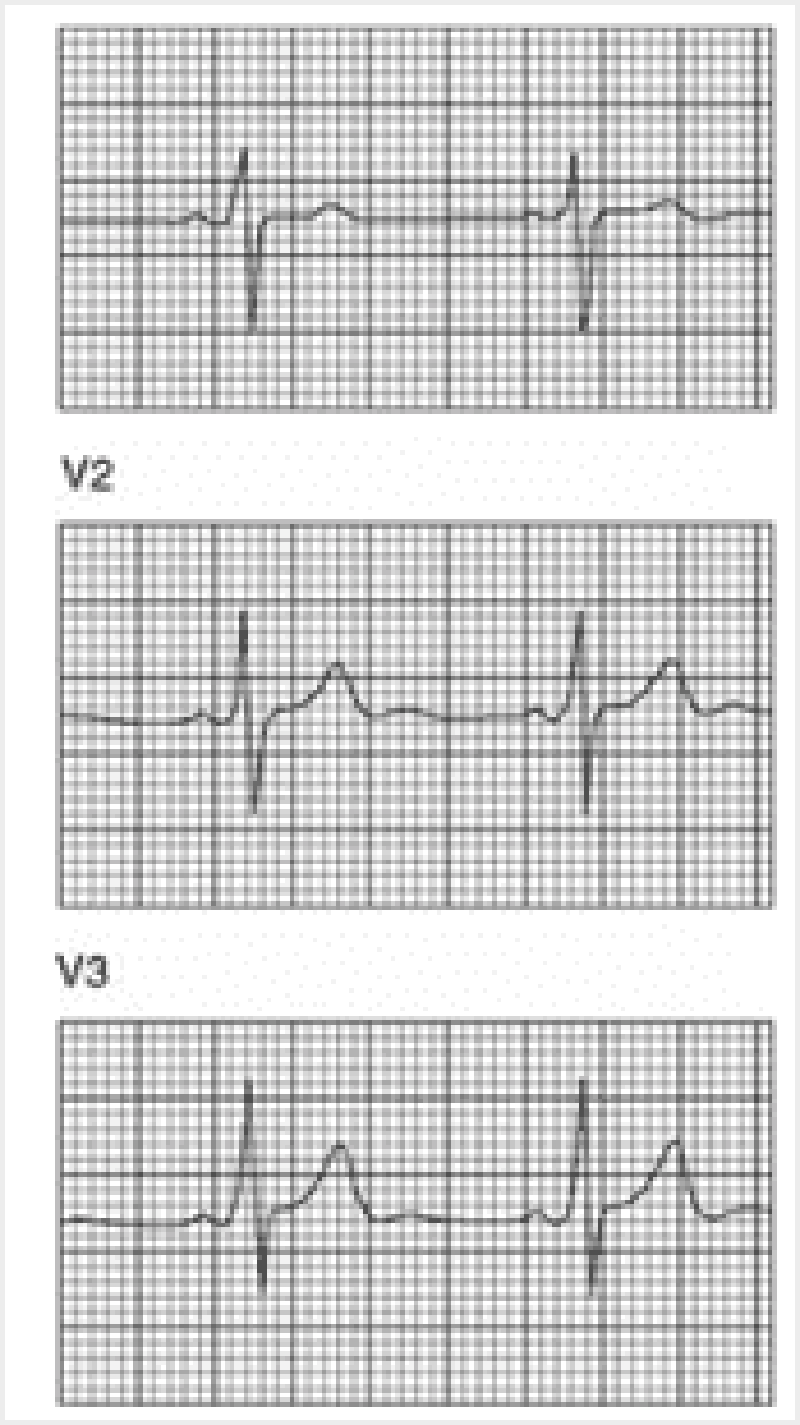
18. You are performing medical screening of new military recruits when an 18-year-old male reports several episodes of palpitation and syncope over the past several years. Physical examination is unremarkable. An ECG is obtained with excerpts shown below. What is the most likely diagnosis?
A. Prior myocardial infarction secondary to coronary artery disease
B. Congenital prolonged QT syndrome
C. Hypertrophic obstructive cardiomyopathy (HOCM)
D. Preexcitation syndrome (Wolff-Parkinson-White)
E. Rheumatic mitral stenosis
19. A 67-year-old male presents to your clinic to establish primary care; he is asymptomatic. He has a history of hypertension for which he takes hydrochlorothiazide. His father had a myocardial infarction at age 62. The patient smoked until 5 years ago, but has been abstinent from tobacco since then. His blood pressure in the office today is 132/78. Aside from being overweight, the remainder of the physical examination is unremarkable. Which of the following preventive health interventions would be most appropriately offered to him today?
A. Carotid ultrasound to evaluate for carotid artery stenosis
B. Abdominal ultrasound to evaluate for aortic aneurysm
C. Lipoprotein(a) assay to evaluate coronary heart disease risk
D. Exercise (treadmill) stress testing to evaluate for coronary artery disease
E. Homocysteine level to evaluate coronary heart disease risk
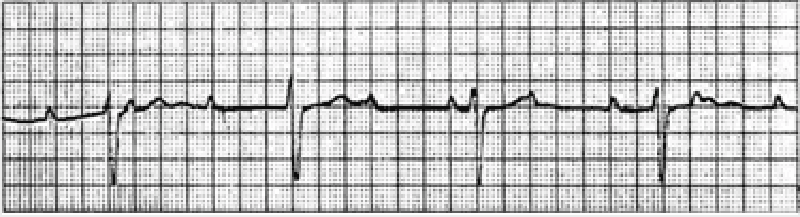
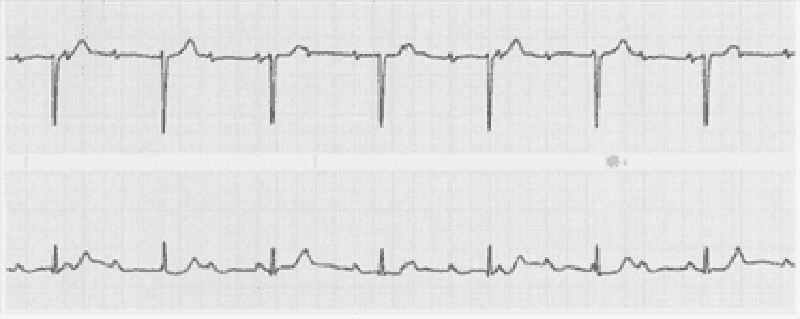
20. You are called by a surgical colleague to evaluate a 54-year-old woman with ECG abnormalities one day after a subtotal thyroidectomy for a toxic multinodular goiter. Her only medication is fentanyl for postoperative pain control. The patient denies any history of syncope, and has no family history of sudden cardiac death. Physical examination is unremarkable except for a clean postoperative incision at the base of the neck. Her ECG is reproduced below. What is the best next step in evaluation and management of this patient?
A. Administration of intravenous magnesium sulfate
B. Measurement of serum ionized calcium
C. Stat noncontrast CT scan of the brain
D. Formal auditory testing
E. Reassure the patient that her ECG is normal for a woman her age
21. A 36-year-old woman presents to the ED with sudden onset of left-sided chest pain and mild shortness of breath that began the night before. She was able to fall asleep without difficulty but woke up in the morning with persistent pain that is worsened upon taking a deep breath. She walked up the stairs at home and became very short of breath, which made her come to the ED. Two weeks ago, she took a 7- hour flight from Europe and since then has left-sided calf pain and swelling. What is the most common ECG finding for this patient’s presentation?
A. S1Q3T3 pattern
B. Atrial fibrillation
C. Right-axis deviation
D. Right-atrial enlargement
E. Tachycardia or nonspecific ST-T–wave changes
22. A 54-year-old woman presents to the ED because of a change in behavior at home. For the past 3 years, she has end-stage renal disease requiring dialysis. Her daughter states that the patient has been increasingly tired and occasionally confused for the past 3 days and has not been eating her usual diet. On examination, the patient is alert and oriented to person only. The remainder of her examination is normal. An initial 12-lead ECG is performed as seen on the following page. Which of the following electrolyte abnormalities best explains these findings?
A. Hypokalemia
B. Hyperkalemia
C. Hypocalcemia
D. Hypercalcemia
E. Hyponatremia
23. A 42-year-old man found vomiting in the street is brought to the ED by emergency medical services (EMS). He has a known history of alcohol abuse with multiple presentations for intoxication. Today, the patient complains of acute onset, persistent chest pain associated with dysphagia, and pain upon flexing his neck. His BP is 115/70 mm Hg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 97% on room air. As you listen to his heart, you hear a crunching sound. His abdomen is soft with mild epigastric tenderness. The ECG is sinus tachycardia without ST-T–wave abnormalities. On chest radiograph, you note lateral displacement of the left mediastinal pleura. What is the most likely diagnosis?
A. Aspiration pneumonia
B. Acute pancreatitis
C. Pericarditis
D. Esophageal perforation
E. Aortic dissection
24. A 65-year-old man with a history of chronic hypertension presents to the ED with sudden-onset tearing chest pain that radiates to his jaw. His BP is 205/110 mm Hg, HR is 90 beats per minute, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. He appears apprehensive. On cardiac examination you hear a diastolic murmur at the right sternal border. A chest x-ray reveals a widened mediastinum. Which of the following is the preferred study of choice to diagnose this patient’s condition?
A. Electrocardiogram (ECG)
B. Transthoracic echocardiography (TTE)
C. Transesophageal echocardiography (TEE)
D. Computed tomography (CT) scan
E. Magnetic resonance imaging (MRI)
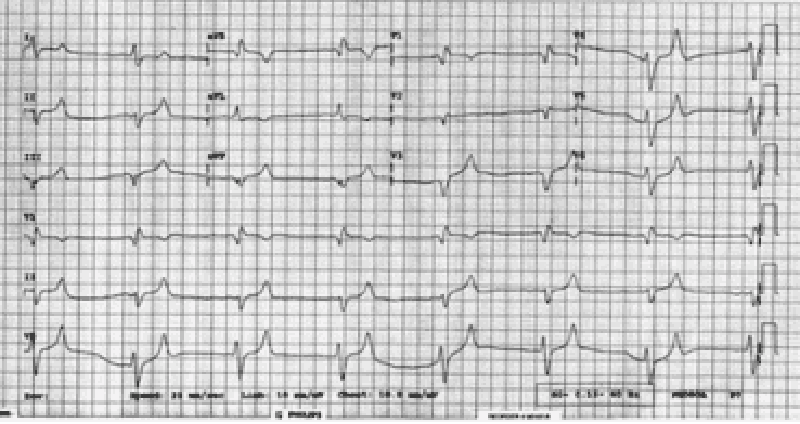
25. A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mm Hg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
A. Anteroseptal
B. Anterior
C. Lateral
D. Inferior
E. Posterior
26. A 21-year-old woman presents to the ED complaining of lightheadedness. Her symptoms appeared 45 minutes ago. She has no other symptoms and is not on any medications. She has a medical history of mitral valve prolapse. Her HR is 170 beats per minute and BP is 105/55 mm Hg. Physical examination is unremarkable. After administering the appropriate medication, her HR slows down and her symptoms resolve. You repeat a 12-lead ECG that shows a rate of 89 beats per minute with a regular rhythm. The PR interval measures 100 milliseconds and there is a slurred upstroke of the QRS complex. Based on this information, which of the following is the most likely diagnosis?
A. Ventricular tachycardia
B. Atrial flutter with 3:1 block
C. Atrial fibrillation
D. Lown-Ganong-Levine (LGL) syndrome
E. Wolff-Parkinson-White (WPW) syndrome
27. A 61-year-old woman with a history of diabetes and hypertension is brought to the ED by her daughter. The patient states that she started feeling short of breath approximately 12 hours ago and then noticed a tingling sensation in the middle of her chest and became diaphoretic. An ECG reveals ST depression in leads II, III, and aVF. You believe that the patient had a non–ST-elevation MI (NSTEMI). Which of the following cardiac markers begins to rise within 3 to 6 hours of chest pain onset, peaks at 12 to 24 hours, and returns to baseline in 7 to 10 days?
A. Myoglobin
B. Creatinine kinase (CK)
C. Creatinine kinase-MB (CK-MB)
D. Troponin I
E. Lactic dehydrogenase (LDH)
28. A 71-year-old man is playing cards with some friends when he starts to feel a pain in the left side of his chest. His fingers in the left hand become numb and he feels short of breath. His wife calls the ambulance and he is brought to the hospital. In the ED, an ECG is performed. Which of the following best describes the order of ECG changes seen in an MI?
A. Hyperacute T wave, ST-segment elevation, Q wave
B. Q wave, ST-segment elevation, hyperacute T wave
C. Hyperacute T wave, Q wave, ST-segment elevation
D. ST-segment elevation, Q wave, hyperacute T wave
E. ST-segment elevation, hyperacute T wave, Q wave
29. While playing a match of tennis, a 56-year-old man with a medical history significant only for acid reflux disease starts to feel substernal chest pain that radiates into his left arm and shortness of breath. His pain feels better after drinking antacid, but since it is not completely resolved, his partner calls 911. Upon arrival, EMS administers aspirin and sublingual nitroglycerin. After 20 minutes, the man’s symptoms resolve. He is brought to the ED for further evaluation where his ECG shows sinus rhythm without any ischemic abnormalities. You order a chest radiograph and send his blood work to the laboratory for analysis. Which of the following statements regarding the diagnosis of acute MI is most accurate?
A. A normal ECG rules out the diagnosis of acute MI.
B. One set of negative cardiac enzymes is sufficient to exclude the diagnosis of MI in this patient.
C. Troponin may not reach peak levels for at least 12 hours.
D. Relief of symptoms by antacids essentially rules out a cardiac cause of his chest pain.
E. Epigastric discomfort and indigestion is a rare presentation of ACS.
30. A 22-year-old college student went to the health clinic complaining of a fever over the last 5 days, fatigue, myalgias, and a bout of vomiting and diarrhea. The clinic doctor diagnosed him with acute gastroenteritis and told him to drink more fluids. Three days later, the student presents to the ED complaining of substernal chest pain that is constant. He also feels short of breath. His temperature is 100.9°F, HR is 119 beats per minute, BP is 120/75 mm Hg, and RR is 18 breaths per minute. An ECG is performed revealing sinus tachycardia. A chest radiograph is unremarkable. Laboratory tests are normal except for slightly elevated WBCs. Which of the following is the most common cause of this patient’s diagnosis?
A. Streptococcus viridans
B. Influenza A
C. Coxsackie B virus
D. Atherosclerotic disease
E. Cocaine abuse
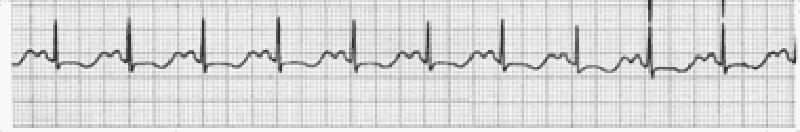
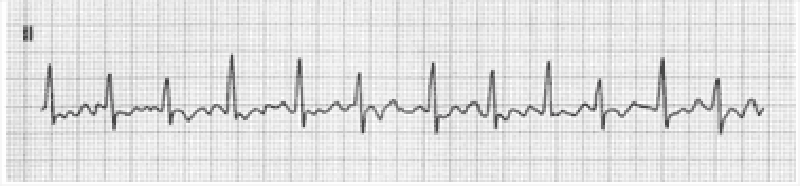
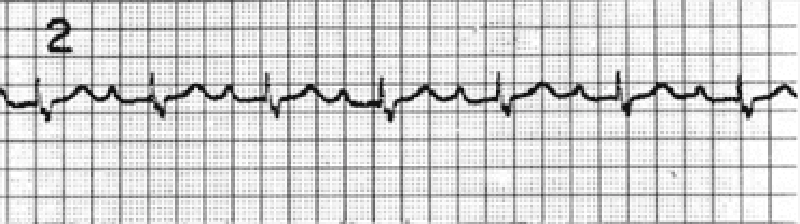
31. A 23-year-old woman who is an elementary school teacher is brought to the ED after syncopizing in her classroom while teaching. Prior to passing out, she describes feeling light- headed and dizzy and next remembers being in the ambulance. There was no evidence of seizure activity. She has no medical problems and does not take any medications. Her father died of a “heart problem” at 32 years of age. She does not smoke or use drugs. BP is 120/70 mm Hg, pulse rate is 71 beats per minute, RR is 14 breaths per minute, and oxygen saturation is 100% on room air. Her physical examination and laboratory results are all normal. A rhythm strip is seen below. Which of the following is the most likely diagnosis?
A. Wolff-Parkinson-White syndrome
B. Long QT syndrome
C. Lown-Ganong- Levine syndrome
D. Complete heart block
E. Atrial flutter
32. A 55-year-old man presents to the ED with chest pain and shortness of breath. His BP is 170/80 mm Hg, HR is 89 beats per minute, and oxygen saturation is 90% on room air. Physical examination reveals crackles midway up both lung fields and a new holosystolic murmur that is loudest at the apex and radiates to the left axilla. ECG reveals ST elevations in the inferior leads. Chest radiograph shows pulmonary edema with a normalsized cardiac silhouette. Which of the following is the most likely cause of the cardiac murmur?
A. Critical aortic stenosis
B. Papillary muscle rupture
C. Pericardial effusion
D. CHF
E. Aortic dissection
33. A 22-year-old man presents to the ED with a history consistent with an acute MI. His ECG reveals ST elevations and his cardiac biomarkers are positive. He has been smoking half a pack of cigarettes per day for the last 3 months. He drinks alcohol when hanging out with his friends. His grandfather died of a heart attack at 80 years of age. The patient does not have hypertension or diabetes mellitus and takes no prescription medications. A recent cholesterol check revealed normal levels of total cholesterol, low- density lipoprotein (LDL), and high-density lipoprotein (HDL). Which of the following is the most likely explanation for his presentation?
A. Cigarette smoking
B. Family history of heart attack at age 80 years
C. Incorrectly placed leads on the ECG
D. Undisclosed cocaine use
E. Alcohol use
34. A 55-year-old man with hypertension and a one-pack-per-day smoking history presents to the ED complaining of three episodes of severe heavy chest pain this morning that radiated to his left shoulder. In the past, he experienced chest discomfort after walking 20 minutes that resolved with rest. The episodes of chest pain this morning occurred while he was reading the newspaper. His BP is 155/80 mm Hg, HR 76 beats per minute, and RR 15 breaths per minute. He does not have chest pain in the ED. An ECG reveals sinus rhythm with a rate of 72. A troponin I is negative. Which of the following best describes this patient’s diagnosis?
A. Variant angina
B. Stable angina
C. Unstable angina
D. Non–ST-elevation MI
E. ST-elevation MI (STEMI)

35. A 58-year-old man is brought to the ED for a syncopal episode at dinner. His wife states that he was well until she found him suddenly slumping in the chair and losing consciousness for a minute. The patient recalls having some chest discomfort and shortness of breath prior to the episode. His rhythm strip, obtained by EMS, is shown below. Which of the following best describes these findings?
A. Mobitz type I
B. Mobitz type II
C. First-degree atrioventricular (AV) block
D. Atrial flutter with premature ventricular contractions (PVCs)
E. Sinus bradycardia
36. In the ICU, a patient suddenly becomes pulseless and unresponsive, with cardiac monitor indicating ventricular tachycardia. The crash cart is immediately available. What is the best first therapy?
A. Amiodarone 150-mg IV push
B. Lidocaine 1.5-mg/kg IV push
C. Epinephrine 1-mg IV push
D. Defibrillation at 200 J
E. Defibrillation at 360 J
37. A 70-year-old female has been healthy except for hypertension treated with a thiazide diuretic. She presents with sudden onset of a severe, tearing chest pain, which radiates to the back and is associated with dyspnea and diaphoresis. Blood pressure is 210/94. Lung auscultation reveals bilateral basilar rales. A faint murmur of aortic insufficiency is heard. The BNP level is elevated at 550 pg/mL (Normal < 100). ECG shows nonspecific ST-T changes. Chest x-ray suggests a widened mediastinum. Which of the following choices represents the best initial management?
A. IV furosemide plus IV loading dose of digoxin
B. Percutaneous coronary intervention with consideration of angioplasty and/or stenting
C. Blood cultures and rapid initiation of vancomycin plus gentamicin, followed by echocardiography
D. IV beta-blocker to control heart rate, IV nitroprusside to control blood pressure, transesophageal echocardiogram
E. IV heparin followed by CT pulmonary angiography
38. A 55-year-old African American female presents to the ER with lethargy and blood pressure of 250/150. Her family members indicate that she was complaining of severe headache and visual disturbance earlier in the day. They report a past history of asthma but no known kidney disease. On physical examination, retinal hemorrhages are present. Which of the following is the best approach?
A. Intravenous labetalol therapy
B. Continuous- infusion nitroprusside
C. Clonidine by mouth to lower blood pressure
D. Nifedipine sublingually to lower blood pressure
E. Intravenous loop diuretic
39. A 36-year-old male presents with the sensation of a racing heart. His blood pressure is 110/70, respiratory rate 14/minute, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia with rate 180, which you correctly diagnose as paroxysmal atrial tachycardia. Carotid massage and Valsalva maneuver do not improve the heart rate. Which of the following is the initial therapy of choice?
A. Adenosine 6-mg rapid IV bolus
B. Verapamil 2.5 to 5 mg IV over 1 to 2 min
C. Diltiazem 0.25-mg/kg IV over 2 min
D. Digoxin 0.5 mg IV slowly
E. Electrical cardioversion at 50 J
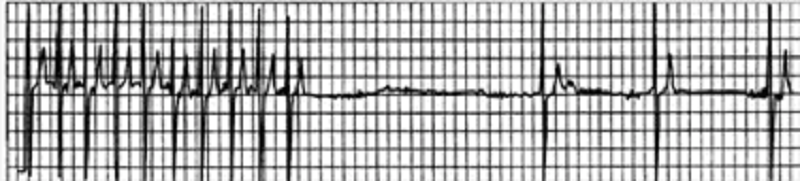
40. A 70-year-old male with a history of mild chronic kidney disease, diabetes mellitus, and CHF is admitted to your inpatient service with decreased urine output, weakness, and shortness of breath. He takes several medications but cannot remember their names. Labs are pending; his ECG is shown below. Based on the information available, what is the best initial step in management?
A. Administration of intravenous insulin
B. Administration of intravenous sodium bicarbonate
C. Administration of intravenous 3% hypertonic saline
D. Administration of oral sodium polystyrene sulfonate
E. Administration of intravenous calcium gluconate
41. A 59-year-old man presents to the emergency department (ED) complaining of new-onset chest pain that radiates to his left arm. He has a history of hypertension, hypercholesterolemia, and a 20-pack-year smoking history. His electrocardiogram (ECG) is remarkable for T-wave inversions in the lateral leads. Which of the following is the most appropriate next step in management?
A. Give the patient two nitroglycerin tablets sublingually and observe if his chest pain resolves.
B. Place the patient on a cardiac monitor, administer oxygen, and give aspirin.
C. Call the cardiac catheterization laboratory for immediate percutaneous coronary intervention (PCI).
D. Order a chest x-ray; administer aspirin, clopidogrel, and heparin.
E. Start a β-blocker immediately.
42. A 51-year-old man with a long history of hypertension presents to the ED complaining of intermittent chest palpitations lasting for a week. He denies chest pain, shortness of breath, nausea, and vomiting. He recalls feeling similar episodes of palpitations a few months ago but they resolved. His blood pressure (BP) is 130/75 mm Hg, heart rate (HR) is 130 beats per minute, respiratory rate (RR) is 16 breaths per minute, and oxygen saturation is 99% on room air. An ECG is seen below. Which of the following is the most appropriate next step in management?
A. Sedate patient for immediate synchronized cardioversion with 100 J.
B. Prepare patient for the cardiac catheterization laboratory.
C. Administer warfarin.
D. Administer amiodarone .
E. Administer diltiazem
43. A 67-year-old woman is brought to the ED by paramedics complaining of dyspnea, fatigue, and palpitations. Her BP is 80/50 mm Hg, HR is 139 beats per minute, and RR is 20 breaths per minute. Her skin is cool and she is diaphoretic. Her lung examination reveals bilateral crackles and she is beginning to have chest pain. Her ECG shows a narrow complex irregular rhythm with a rate in the 140s. Which of the following is the most appropriate immediate treatment for this patient?
A. Diltiazem
B. Metoprolol
C. Digoxin
D. Coumadin
E. Synchronized cardioversion
44. A 61-year-old woman with a history of congestive heart failure (CHF) is at a family picnic when she starts complaining of shortness of breath. Her daughter brings her to the ED where she is found to have an oxygen saturation of 85% on room air with rales halfway up both of her lung fields. Her BP is 185/90 mm Hg and pulse rate is 101 beats per minute. On examination, her jugular venous pressure (JVP) is 6 cm above the sternal angle. There is lower extremity pitting edema. Which of the following is the most appropriate first-line medication to lower cardiac preload?
A. Metoprolol
B. Morphine sulfate
C. Nitroprusside
D. Nitroglycerin
E. Oxygen
45. A 27-year-old man complains of chest palpitations and lightheadedness for the past hour. He has no past medical history and is not taking any medications. He drinks a beer occasionally on the weekend and does not smoke cigarettes. His HR is 180 beats per minute, BP is 110/65 mm Hg, and oxygen saturation is 99% on room air. An ECG reveals an HR of 180 beats per minute with a QRS complex of 90 milliseconds with a regular rhythm. There are no discernable P waves. Which of the following is the most appropriate medication to treat this dysrhythmia?
A. Digoxin
B. Lidocaine
C. Amiodarone
D. Adenosine
E. Bretylium

46. A 59-year-old man presents to the ED with left-sided chest pain and shortness of breath that began 1 hour ago. Initial vital signs are BP 85/45 mm Hg, HR 105 beats per minute, RR 20 breaths per minute, and oxygen saturation 94% on room air. An ECG is seen below. Which of the following is the most appropriate definitive treatment?
A. Administer metoprolol or diltiazem
B. Electrical cardioversion
C. Administer calcium gluconate
D. Thrombolytic therapy
E. Percutaneous angioplasty
47. A 63-year-old insurance agent is brought to the ED by paramedics for shortness of breath and an RR of 31 breaths per minute. The patient denies chest pain, fever, vomiting, or diarrhea. His wife says he ran out of his “water pil ” 1 week ago. His BP is 185/90 mm Hg, HR is 101 beats per minute, oxygen saturation is 90% on room air, and temperature is 98.9°F. There are crackles midway up both lung fields and 2+ pitting edema midway up his legs. An ECG shows sinus tachycardia. The patient is sitting up and able to speak to you. After placing the patient on a monitor and inserting an IV, which of the following is the most appropriate next step in management?
A. Obtain blood cultures and complete blood cell (CBC) count, and begin empiric antibiotic therapy.
B. Order a statim (STAT) portable chest x-ray.
C. Administer oxygen via nasal cannula and have the patient chew an aspirin.
D. Administer oxygen via non-rebreather, furosemide, nitroglycerin, and consider noninvasive respiratory therapy.
E. Rapid sequence endotracheal intubation.
48. A 62-year-old woman presents to the ED with general weakness, shortness of breath, and substernal chest pain that radiates to her left shoulder. Her BP is 155/80 mm Hg, HR is 92 beats per minute, and RR is 16 breaths per minute. You suspect that she is having an acute MI. Which of the following therapeutic agents has been shown to independently reduce mortality in the setting of an acute MI?
A. Nitroglycerin
B. Aspirin
C. Unfractionated heparin
D. Lidocaine
E. Diltiazem
49. A 57-year-old man complains of chest palpitations and light-headedness for the past hour. Five years ago he underwent a cardiac catheterization with coronary artery stent placement. He smokes half a pack of cigarettes daily and drinks a glass of wine at dinner. His HR is 140 beats per minute, BP is 115/70 mm Hg, and oxygen saturation is 99% on room air. An ECG reveals a wide complex tachycardia at a rate of 140 that is regular in rhythm. An ECG from 6 months ago shows a sinus rhythm at a rate of 80. Which of the following is the most appropriate medication to treat this dysrhythmia?
A. Digoxin
B. Diltiazem
C. Amiodarone
D. Adenosine
E. Bretylium

50. As you are examining the patient described in the previous question, he starts to complain of chest discomfort and shortness of breath and has another syncopal episode. His ECG is shown below. Which of the following is the most appropriate next step in management?
A. Call cardiology consult
B. Cardiovert the patient
C. Administer metoprolol
D. Administer amiodarone
E. Apply transcutaneous pacemaker
51. You have been asked to evaluate a 42-year-old white male smoker who presented to the emergency department with sudden onset of crushing substernal chest pain, nausea, diaphoresis and shortness of breath. His initial ECG revealed ST segment elevation in the anterior-septal leads. Cardiac enzymes were normal. The patient underwent emergent cardiac catheterization, which revealed only a 25% stenosis of the left anterior descending (LAD) artery. No percutaneous intervention was performed. Which of the following interventions would most likely reduce his risk of similar episodes in the future?
A. Placement of a percutaneous drug-eluting coronary artery stent.
B. Placement of a percutaneous non-drug-eluting coronary artery stent.
C. Beginning therapy with an ACE inhibitor.
D. Beginning therapy with a beta-blocker.
E. Beginning therapy with a calcium-channel blocker.
52. A 15-year-old male presents to your office on the advice of his football coach. The patient started playing football this year and suffered a syncopal episode at practice yesterday. He reports that he was sprinting with the rest of the team and became lightheaded. He lost consciousness and fell to the ground, regaining consciousness within one or two minutes. He suffered no trauma during the event. He has no prior history of head injury or recent illness. He has had no prior episodes of syncope. The patient is adopted and family history unavailable. Physical examination is unremarkable. What is the best course of action regarding this patient’s syncopal episode?
A. Perform an ECG and echocardiogram. The patient may not return to competitive sports until results are available.
B. Perform an ECG. The patient may not return to competitive sports until results are available.
C. Perform an ECG. The patient may return to competitive sports pending the results.
D. Reassurance. The patient may return to competitive sports provided he increases his water consumption during practice times.
E. Reassurance. The patient may return to competitive sports with no restrictions
53. An 82-year-old white female is admitted to the hospital for observation after presenting to the emergency department with dizziness. After being placed on a cardiac monitor in the ER, the rhythm strip below was recorded. There is no past history of cardiac disease, diabetes, or hypertension. With prompting, the patient discloses several prior episodes of transient dizziness and one episode of brief syncope in the past. Physical examination is unremarkable. Which of the following is the best plan of care?
A. Reassurance. This is a benign condition, and no direct therapy is needed.
B. Reassurance. The patient may not drive until she is symptom free, but otherwise no direct therapy is needed.
C. Nuclear cardiac stress testing; treatment depending on results.
D. Begin therapy with aspirin.
E. Arrange placement of a permanent pacemaker
54. Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to your office concerned about low-grade fever and pleuritic chest pain. There is no associated shortness of breath. Lungs are clear to auscultation and the heart is free of murmur, gallop, or rub. ECG is unchanged from the last one in the hospital. Which therapy is most likely to be effective?
A. Antibiotics
B. Anticoagulation with warfarin (Coumadin)
C. An anti-inflammatory agent
D. An increase in antianginal medication
E. An anxiolytic agent
55. A 55-year-old patient presents to you after a 3-day hospital stay for gradually increasing shortness of breath and leg swelling while away on a business trip. He was told that he had congestive heart failure, but is asymptomatic now, with normal vital signs and physical examination. An echocardiogram shows an estimated ejection fraction of 38%. The patient likes to keep medications to a minimum. He is currently on aspirin and simvastatin. Which would be the most appropriate additional treatment?
A. Begin an ACE inhibitor and then add a beta-blocker on a scheduled basis.
B. Begin digoxin plus furosemide on a scheduled basis.
C. Begin spironolactone on a scheduled basis.
D. Begin furosemide plus nitroglycerin.
E. Given his preferences, no other medication is needed unless shortness of breath and swelling recur.
56. A 34-year-old woman is referred by an OB-GYN colleague for the onset of fatigue and dyspnea on exertion 1 month after her second vaginal delivery. Physical examination reveals a laterally displaced PMI, elevated jugular venous pressure and 2+pitting lower extremity edema. Echocardiogram shows systolic dysfunction with an ejection fraction of 30%. Which statement most accurately describes her condition?
A. This disease may occur unexpectedly years after pregnancy and delivery.
B. About half of similar patients will recover completely.
C. The condition is idiosyncratic; the risk of recurrence with a future pregnancy is no greater than average.
D. This condition will require a different therapeutic approach than the typical dilated cardiomyopathy.
E. This condition will require endomyocardial biopsy for diagnosis.
57. A 72-year-old Caucasian male presents with shortness of breath that awakens him at night. At baseline he is able to walk less than a block before stopping to catch his breath. Physical examination findings include bilateral basilar rales and neck vein distention. The patient has a known history of congestive heart failure, and his last echocardiogram revealed an ejection fraction of 25%. The patient is compliant with a medication regimen including an ACE inhibitor, beta-blocker, and loop diuretic. Blood pressure is well controlled. What additional treatment should you begin next?
A. Spironolactone
B. Aspirin
C. Amlodipine
D. Warfarin
E. Hydralazine and isosorbide dinitrate
58. A 68-year-old male was intubated in the emergency room because of pulmonary edema. Stat echocardiogram reveals an ejection fraction of 45% and severe mitral regurgitation. In spite of aggressive diuresis with furosemide, the patient continues to require mechanical ventilation secondary to pulmonary edema. What is the best next step in treating this patient?
A. Arrange for mitral valve replacement surgery.
B. Place an intra-aortic balloon pump.
C. Begin metoprolol.
D. Begin a second loop diuretic.
E. Begin intravenous enalapril
59. A 30-year-old female presents with a chief complaint of palpitations. A 24-hour Holter monitor shows occasional unifocal premature ventricular contractions and premature atrial contractions. Which of the following is the best management for this patient?
A. Anxiolytic therapy
B. Beta-blocker therapy
C. Digoxin
D. Quinidine
E. Reassurance, no medication
60. An active 78-year-old female with history of hypertension presents with the new onset of left hemiparesis. Cardiac monitoring reveals atrial fibrillation. She had been in sinus rhythm on check-up 3 months earlier. Optimal management at discharge includes a review of antihypertensive therapy, a ventricular rate control agent, and which of the following?
A. Automated implanted cardioverter-defibrillator (AICD)/permanent pacemaker to avoid the need for anticoagulation
B. Immediate direct-current cardioversion
C. Antiplatelet therapy such as aspirin, without warfarin
D. Antiplatelet therapy plus warfarin with a target INR of 1.5
E. Warfarin with a target INR of 2.0 to 3.0.
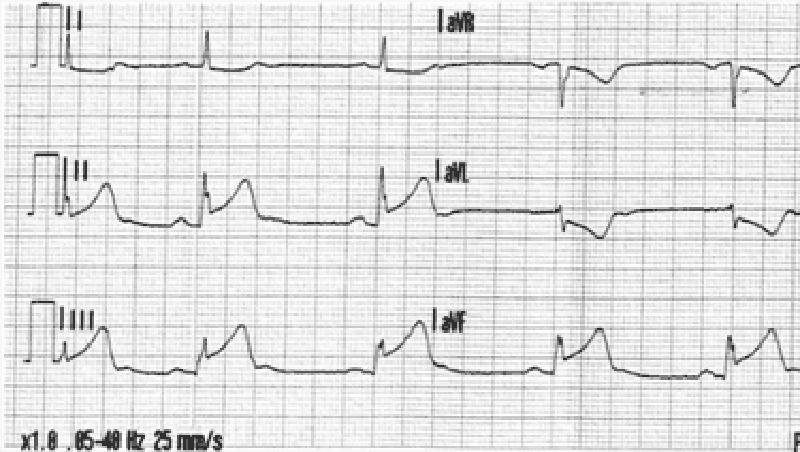
61. A 72-year-old male with a history of poorly controlled hypertension develops a viral upper respiratory infection. On his second day of symptoms he experiences palpitations and presents to the emergency room. His blood pressure is 118/78. The following rhythm strip is obtained. What is the best next step in the management of this patient?
A. Administration of intravenous metoprolol
B. Administration of intravenous adenosine
C. Administration of intravenous amiodarone
D. Emergent electrical cardioversion
E. Initiation of chest compressions and preparation for semielective intubation
62. An otherwise asymptomatic 65-year-old man with diabetes presents to the ER with a sports-related right shoulder injury. His heart rate is noted to be irregular, and this ECG is obtained. Which of the following is the best immediate therapy?
A. Atropine
B. Isoproterenol
C. Pacemaker placement
D. Electrical cardioversion
E. Observation
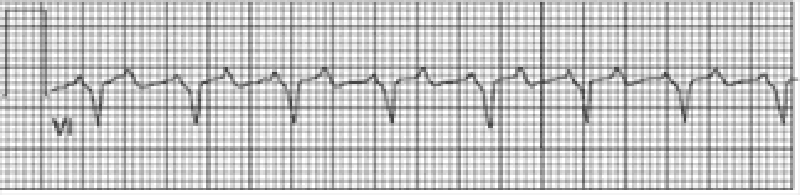
63. A patient has been in the coronary care unit for the past 24 hours with an acute anterior myocardial infarction. He develops the abnormal rhythm shown below, although blood pressure remains stable at 110/68. Which of the following is the best next step in therapy?
A. Perform cardioversion.
B. Arrange for pacemaker placement.
C. Give digoxin.
D. Give propranolol.
E. Give lidocaine
64. A 70-year-old male with a history of coronary artery disease presents to the emergency department with 2 hours of substernal chest pressure, diaphoresis, and nausea. He reports difficulty “catching his breath.” An electrocardiogram shows septal T-wave inversion. The patient is given 325-mg aspirin and sublingual nitroglycerin while awaiting the results of his blood work. His troponin I is 0.65 ng/mL (normal < 0.04 ng/mL). The physician in the emergency department starts the patient on low-molecular- weight heparin. His pain is 3/10. Blood pressure is currently 154/78 and heart rate is 72. You are asked to assume care of this patient. What is the best next step in management?
A. Arrange for emergent cardiac catheterization.
B. Begin intravenous thrombolytic therapy.
C. Admit the patient to a monitored cardiac bed and repeat cardiac enzymes and ECG in 6 hours.
D. Begin intravenous beta-blocker therapy.
E. Begin clopidogrel 300 mg po each day.
65. You are volunteering with a dental colleague in a community indigent clinic. A nurse has prepared a list of patients who are scheduled for a dental procedure and may need antibiotic prophylaxis beforehand. Of the patients listed below, who would be most likely to benefit from antibiotic prophylaxis to prevent infective endocarditis?
A. 17-year-old male with coarctation of the aorta
B. 26-year-old female with a ventricular septal defect repaired in childhood
C. 42-year-old female with mitral valve prolapse
D. 65-year-old male with prosthetic aortic valve
E. 72-year-old female with aortic stenosis
66. An 80-year-old woman was admitted to your service for dizziness. Cardiac monitoring initially revealed atrial fibrillation with rapid ventricular response. Her ventricular rate was controlled with beta-blocker. An echocardiogram revealed an enlarged left atrium and an ejection fraction of 50%. No evidence of diastolic heart dysfunction was noted. She is now asymptomatic, with blood pressure 130/80, heart rhythm irregularly irregular, and heart rate around 80/minute. Which of the following is the best management strategy of this patient’s arrhythmia?
A. Electrical cardioversion plus prolonged anticoagulation
B. Electrical cardioversion without anticoagulation
C. Chemical cardioversion plus prolonged anticoagulation
D. Chemical cardioversion without anticoagulation
E. Continued rate control plus prolonged anticoagulation
67. You are seeing a 45-year-old female patient of your partner for the first time in your clinic. A quick review of the patient’s medical record shows that her systolic blood pressure was greater than 140 mm Hg at both of her last clinic appointments. Her medical history is otherwise significant only for diabetes mellitus. Her blood pressure today is 164/92. What is the best next step in her blood pressure management?
A. Ask the patient to keep a written record of her blood pressure and bring with her to a return appointment.
B. Advise the patient to begin a heart healthy, low sodium diet and refer to a nutritionist.
C. Prescribe an ACE inhibitor in addition to heart healthy diet.
D. Prescribe a dihydropyridine calcium-channel blocker in addition to a heart healthy diet.
E. Arrange for echocardiogram to assess for end-organ damage
68. A 68-year-old male complains of pain in his calves while walking. He notes bilateral foot pain, which awakens him at night. His blood pressure is 117/68. Physical examination reveals diminished bilateral lower extremity pulses. An ankle: brachial index measures 0.6. The patient’s current medications include aspirin and hydrochlorothiazide. Which of the following is the best initial management plan for this patient’s complaint?
A. Smoking cessation therapy, warfarin
B. Smoking cessation therapy, graduated exercise regimen, cilostazol
C. Smoking cessation therapy, schedule an arteriogram
D. Smoking cessation therapy, warfarin, peripherally acting calcium-channel blocker
E. Smoking cessation therapy, consultation with a vascular surgeon
69. A 29-year-old tall, thin man presents to the ED after feeling short of breath for 2 days. In the ED, he is in no acute distress. His BP is 115/70 mm Hg, HR is 81 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 98% on room air. Cardiac, lung, and abdominal examinations are normal. An ECG reveals sinus rhythm at a rate of 79. A chest radiograph shows a small right-sided (< 10% of the hemithorax) spontaneous pneumothorax. A repeat chest x-ray 6 hours later reveals a decreased pneumothorax. Which of the following is the most appropriate next step in management?
Discharge the patient with follow-up in 24 hours.
Perform needle decompression in the second intercostal space, midclavicular line.
Insert a 20F chest tube into right hemithorax
Observe for another 6 hours
Admit for pleurodesis
70. A 47-year-old man with a history of hypertension presents to the ED complaining of continuous left-sided chest pain that began while snorting cocaine 1 hour ago. The patient states he never experienced chest pain in the past when using cocaine. His BP is 170/90 mm Hg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 98% on room air. The patient states that the only medication he takes is alprazolam to “calm his nerves.” Which of the following medications is contraindicated in this patient?
Metoprolol
Diltiazem
Aspirin
Lorazepam
Nitroglycerin
71. A 32-year-old woman presents to the ED with a persistent fever of 101°F over the last 3 days. The patient states that she used to work as a convenience store clerk but was fired 2 weeks ago. Since then, she has been using drugs intravenously daily. Cardiac examination reveals a heart murmur. Her abdomen is soft and nontender with an enlarged spleen. Chest radiograph reveals multiple patchy infiltrates in both lung fields. Laboratory results reveal white blood cells (WBC) 14,000/μL with 91% neutrophils, hematocrit 33%, and platelets 250/μL. An ECG reveals sinus rhythm with first-degree heart block. Which of the following is the most appropriate next step in management?
Obtain four sets of blood cultures, order a TTE, and start antibiotic treatment
Order a monospot test and recommend that the patient refrain from vigorous activities for 1 month
Administer a nonsteroidal anti-inflammatory drug (NSAID) and inform the patient she has pericarditis.
Administer isoniazid (INH) and report the patient to the Department of Health.
Order a Lyme antibody and begin antibiotic therapy.
72. A 31-year-old man who works for a moving company presents to the ED because he thinks he was having a heart attack. He does not smoke, and jogs 3 days a week. His father died of a heart attack in his sixties. He describes a gradual onset of chest pain that is worse with activity and resolves when he is at rest. His HR is 68 beats per minute, BP is 120/70 mm Hg, and RR is 14 breaths per minute. On examination, his lungs are clear and there is no cardiac murmur. You palpate tenderness over the left sternal border at the third and fourth ribs. An ECG reveals sinus rhythm at a rate of 65. A chest radiograph shows no infiltrates or pneumothorax. Which of the following is the most appropriate next step in management?
Administer aspirin and send for a troponin.
Administer aspirin, clopidogrel, and heparin, and admit for acute coronary syndrome (ACS).
Administer ibuprofen and reassure the patient that he is not having a heart attack.
Inject corticosteroid into the costochondral joint to reduce inflammation.
Observe the patient for 6 hours.
73. A 55-year-old man presents to the ED with worsening weakness, muscle cramps, and paresthesias. His past medical history is significant for hypertension and diabetes. He smokes one pack of cigarettes per day. On examination, the patient is alert and oriented and diffusely weak. An ECG is seen below. Which of the following is the most important next step in management?
Administer calcium gluconate
Administer insulin and dextrose
Administer aspirin and call the catheterization laboratory
Order an emergent head CT scan and get a neurology consult.
Collect a sample of his urine to test for ketones.
74. A 59-year-old man presents to the ED with left-sided chest pain and shortness of breath that began 2 hours prior to arrival. He states the pain is pressure-like and radiates down his left arm. He is diaphoretic. His BP is 160/80 mm Hg, HR 86 beats per minute, and RR 15 breaths per minute. ECG reveals 2-mm ST-segment elevation in leads I, aVL, and V 3 to V 6. Which of the following is an absolute contraindication to receiving thrombolytic therapy?
Systolic BP (SBP) greater than 180 mm Hg
Patient on Coumadin and aspirin
Total hip replacement 3 months ago
Peptic ulcer disease
Previous hemorrhagic stroke
75. A 27-year-old man who is otherwise healthy presents to the ED with a laceration on his thumb that he sustained while cutting a bagel. You irrigate and repair the wound and are about to discharge the patient when he asks you if he can receive an ECG. It is not busy in the ED so you perform the ECG, as seen below. Which of the following is the most appropriate next step in management?
Admit the patient for placement of a pacemaker
Admit the patient for a 24-hour observation period.
Administer aspirin and send cardiac biomarkers.
Repeat the ECG because of incorrect lead placement
Discharge the patient home.
76. A 55-year-old man presents to the ED at 2:00 AM with left-sided chest pain that radiates down his left arm. He takes a β-blocker for hypertension, a proton pump inhibitor for gastroesophageal reflux disease, and an antilipid agent for high cholesterol. He also took sildenafil the previous night for erectile dysfunction. His BP is 130/70 mm Hg and HR is 77 beats per minute. Which of the following medications is contraindicated in this patient?
Aspirin
Unfractionated heparin
Nitroglycerin
Metoprolol
Morphine sulphate
77. A 31-year-old kindergarten teacher presents to the ED complaining of acute-onset substernal chest pain that is sharp in nature and radiates to her back. The pain is worse when she is lying down on the stretcher and improves when she sits up. She smokes cigarettes occasionally and was told she has borderline diabetes. She denies any recent surgeries or long travel. Her BP is 145/85 mm Hg, HR is 99 beats per minute, RR is 18 breaths per minute, and temperature is 100.6°F. Examination of her chest reveals clear lungs and a friction rub. Her abdomen is soft and nontender to palpation. Her legs are not swollen. Chest radiography and echocardiography are unremarkable. Her ECG is shown below. Which of the following is the most appropriate next step in management?
Anticoagulate and CT scan to evaluate for a PE
Prescribe a NSAID and discharge the patient
Aspirin, heparin, clopidogrel, and admit for ACS.
Administer thrombolytics if the pain persists
Prescribe antibiotics and discharge the patient.
78. A 51-year-old woman presents to the ED after 5 consecutive days of crushing substernal chest pressure that woke her up from sleep in the morning. The pain resolves spontaneously after 20 to 30 minutes. She is an avid rock climber and jogs 5 miles daily. She has never smoked cigarettes and has no family history of coronary disease. In the ED, she experiences another episode of chest pain. An ECG reveals ST-segment elevations and cardiac biomarkers are negative. The pain is relieved with sublingual nitroglycerin. She is admitted to the hospital and diagnostic testing reveals minimal coronary atherosclerotic disease. Which of the following is the most appropriate medication to treat this patient’s condition?
Aspirin
Calcium channel blocker (CCB)
β-Blocker
H2-Blocker
Antidepressant
79. While discussing a case presentation with a medical student, a nearby patient who just returned from getting an ankle radiograph done yells out in pain. You walk over to him and ask what is wrong. He states that since returning from the radiology suite, his automatic implantable cardioverter defibrillator (AICD) is discharging. You hook him up to the monitor and note that his rhythm is sinus. You observe a third shock while the patient is in sinus rhythm. Which of the following is the most appropriate next step in management?
Send the patient back to the radiology suite for another radiograph to desensitize his AICD.
Administer pain medication and wait until the device representative arrives at the hospital to power off the AICD.
Admit the patient to the telemetry unit to monitor his rhythm and find the cause of his AICD discharge.
Place a magnet over the AICD generator to inactivate it and thereby prevent further shocks
Make a small incision over his chest wall and remove the AICD generator and leads.
80. An 82-year-old woman is brought to the ED by her daughter for worsening fatigue, dizziness, and light-headedness. The patient denies chest pain or shortness of breath. She has not started any new medications. Her BP is 140/70 mm Hg, HR is 37 beats per minute, and RR is 15 breaths per minute. An IV is started and blood is drawn. An ECG is seen below. Which of the following is the most appropriate next step in management?
Bed rest for the next 48 hours and follow-up with her primary-care physician
Administer aspirin, order a set of cardiac enzymes, and admit to the cardiac care unit (CCU).
Place a magnet on her chest to turn off her pacemaker
Admit for Holter monitoring and echocardiogram
Place on a cardiac monitor, place external pacing pads on the patient, and admit to the CCU.
81. 20-year-old woman complains of skin problems and is noted to have erythematous papules on her face with blackheads (open comedones) and whiteheads (closed comedones). She has also had cystic lesions. She is prescribed topical tretinoin, but without a totally acceptable result. You are considering oral antibiotics, but the patient requests oral isotretinoin, which several of her college classmates have used with benefit. Which of the following statements is correct?
Intralesional triamcinolone should be avoided due to its systemic effects
Systemically administered isotretinoin therapy cannot be considered unless concomitant contraceptive therapy is provided.
Antimicrobial therapy is of no value since bacteria are not part of the pathogenesis of the process.
The teratogenic effects of isotretinoin are its only clinically important side effects.
The patient will not benefit from topical antibiotics since she did not respond to topical retinoids.
82. A 22-year-old male presents with a 6-month history of a red, nonpruritic rash over the trunk, scalp, elbows, and knees. These eruptions are more likely to occur during stressful periods and have occurred at sites of skin injury. The patient has tried topical hydrocortisone without benefit. On examination, sharply demarcated plaques are seen with a thick scale. Pitting of the fingernails is present. There is no evidence of synovitis. What is the best first step in the therapy of this patient’s skin disease?
Photochemotherapy (PUVA)
Oral methotrexate
Topical calcipotriene
Oral cyclosporine
Topical fluticasone
83. A 25-year-old complains of fever and myalgias for 5 days and now has developed a macular rash over his palms and soles with some petechial lesions. The patient recently returned from a summer camping trip in Tennessee. Which of the following is the most likely cause of the rash?
Contact dermatitis
Sexual exposure
Tick exposure
Contaminated water
Undercooked pork
84. A 17-year-old female presents with a pruritic rash localized to the wrist. Papules and vesicles are noted in a band like pattern, with slight oozing from some lesions. Which of the following is the most likely cause of the rash?
Herpes simplex
Shingles
Atopic dermatitis
Seborrheic dermatitis
Contact dermatitis
85. A 35-year-old woman develops an itchy rash over her back, legs, and trunk several hours after swimming in a lake. Erythematous, edematous papules and plaques are noted. The wheals vary in size. There are no mucosal lesions and no swelling of the lips. What is the best first step in management of her symptomatic rash?
Subcutaneous epinephrine
Intravenous glucocorticoids
Oral antihistamines (H1 blockers)
Aspirin
Oral doxycycline
86. A 64-year-old woman presents with diffuse hair loss. She says that her hair is “coming out by the handfuls” after shampooing. She was treated for severe community-acquired pneumonia 2 months ago but has regained her strength and is exercising regularly. She is taking no medications. Examination reveals diffuse hair loss. Several hairs can be removed by gentle tugging. The scalp is normal without scale or erythema. Her general examination is unremarkable; in particular, her vital signs are normal, she has no pallor or inflammatory synovitis, and her reflexes are normal with a normal relaxation phase. What is the best next step in her management?
Reassurance
Measurement of serum testosterone and DHEA-S levels
Topical minoxidil
Topical corticosteroids
CBC and antinuclear antibodies
87. A 30-year-old black female has a 2-month history of nonproductive cough and a painful skin eruption in the lower extremities. She denies fever or weight loss. Physical examination shows several nontender raised plaques around the nares and scattered similar plaques around the base of the neck. In the lower extremities she has several erythematous tender nonulcerated nodules, measuring up to 4 cm in diameter. Chest x-ray reveals bilateral hilar adenopathy and a streaky interstitial density in the right upper lobe. What is the best way to establish a histological diagnosis?
Punch biopsy of one of the plaques on the neck
Incisional biopsy of one of the lower extremity nodules
Sputum studies for AFB and fungi
Mediastinoscopy and biopsy of one of the hilar or mediastinal nodes
Serum angiotensin-converting enzyme assay
88. A 72-year-old woman presents with pruritus for the past 6 weeks. She is careful to moisturize her skin after her daily shower and uses soap sparingly. She has never had this symptom before. The itching is diffuse and keeps her awake at night. Over this time, she has lost 15 lb of weight and has noticed diminished appetite. She has previously been healthy and takes no medications. Physical examination shows no evidence of rash; a few excoriations are present. She appears fatigued and shows mild temporal muscle wasting. The general examination is otherwise unremarkable. What is the best next step in her management?
Topical corticosteroids
Oral antihistamines
Psychiatric referral for management of depression
Skin biopsy at the edge of one of the excoriations
Laboratory testing including CBC, comprehensive metabolic panel, and thyroid studies
89. A 53-year-old female presents to the clinic with an erythematous lesion on the dorsum of her right hand. The lesion has been present for the past 7 months and has not responded to corticosteroid treatment. She is concerned because the lesion occasionally bleeds and has grown in size during the past few months. On physical examination you notice an 11-mm erythematous plaque with a small central ulceration. The skin is also indurated with mild crusting on the surface. Which of the following is true about this process?
It is a malignant neoplasm of the keratinocytes with the potential to metastasize
It is an allergic reaction resulting from elevation of serum IgE.
It is a chronic inflammatory condition, which can be complicated by arthritis of small and medium-sized joints.
It is a malignant neoplasm of the melanocytes with the potential to metastasize.
It is the most common skin cancer.
89. A 53-year-old female presents to the clinic with an erythematous lesion on the dorsum of her right hand. The lesion has been present for the past 7 months and has not responded to corticosteroid treatment. She is concerned because the lesion occasionally bleeds and has grown in size during the past few months. On physical examination you notice an 11-mm erythematous plaque with a small central ulceration. The skin is also indurated with mild crusting on the surface. Which of the following is true about this process?
It is a malignant neoplasm of the keratinocytes with the potential to metastasize
It is an allergic reaction resulting from elevation of serum IgE.
It is a chronic inflammatory condition, which can be complicated by arthritis of small and medium-sized joints.
It is a malignant neoplasm of the melanocytes with the potential to metastasize
It is the most common skin cancer
90. A 50-year-old woman develops pink macules and papules on her hands and forearms in association with a sore throat. The lesions are target like, with the centers a dusky violet. What causes of this disorder are most likely in this patient?
Tampons and superficial skin infections
Drugs and herpesvirus infections
Rickettsial and fungal infections
Anxiety and emotional stress
Harsh soaps and drying agents
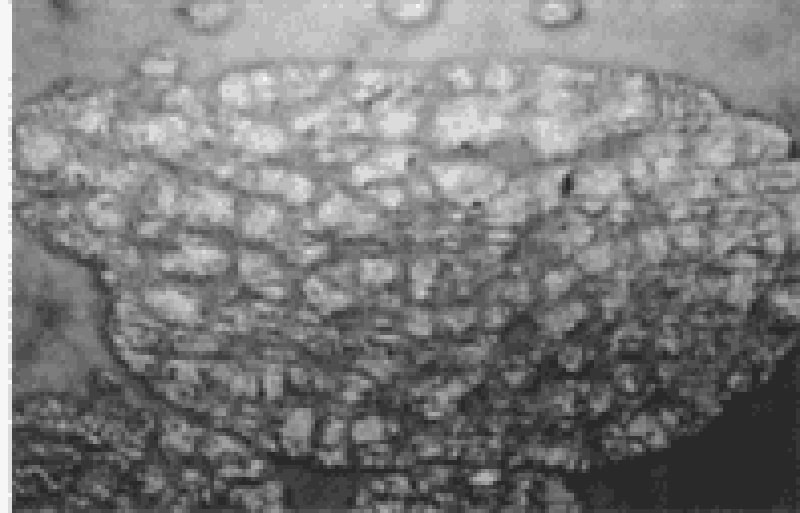
91. A 25-year-old female with blonde hair and fair complexion complains of a mole on her upper back. The lesion is 8 mm in diameter, darkly pigmented, and asymmetric, with an irregular border (see illustration below). Which of the following is the best next step in management?
Tell the patient to avoid sunlight.
Follow the lesion for any evidence of growth.
Obtain metastatic workup.
Obtain full-thickness excisional biopsy.
Obtain shave biopsy.
92. A 39-year-old male with a prior history of myocardial infarction complains of yellow bumps on his elbows and buttocks. Yellow-colored cutaneous plaques are noted in those areas. The lesions occur in crops and have a surrounding reddish halo. Which of the following is the best next step in evaluation of this patient?
Biopsy of skin lesions
Lipid profile
Uric acid level
Chest x-ray
Liver enzymes
93. A 15-year-old girl complains of low-grade fever, malaise, conjunctivitis, runny nose, and cough. After this prodromal phase, a rash of discrete pink macules begins on her face and extends to her hands and feet. She is noted to have small red spots on her palate. What is the most likely cause of her rash?
Toxic shock syndrome
Gonococcal bacteremia
Reiter syndrome
Rubeola (measles)
Rubella (German measles)
94. A 17-year-old girl noted a 2-cm annular pink, scaly lesion on her back. Over the next 2 weeks she develops several smaller oval pink lesions with a fine collarette of scale. They seem to run in the body folds and mainly involve the trunk, although a few occur on the upper arms and thighs. There is no adenopathy and no oral lesions. Which of the following is the most likely diagnosis?
Tinea versicolor
Psoriasis
Lichen planus
Pityriasis rosea
Secondary syphilis
95. A 45-year-old man with Parkinson disease has macular areas of erythema and scaling behind the ears and on the scalp, eyebrows, glabella, nasolabial folds, and central chest. Which of the following is the most likely diagnosis?
Tinea versicolor
Psoriasis
Seborrheic dermatitis
Atopic dermatitis
Dermatophyte infection
96. A 20-year-old white man notes an uneven tan on his upper back and chest. On examination, he has many circular, lighter macules with a barely visible scale that coalesce into larger areas. Which test is most likely to establish the diagnosis?
Punch biopsy
Potassium hydroxide (KOH) microscopic examination
Dermatophyte test medium (DTM) culture for fungus
Serological test for syphilis
Tzanck smear
97. A 33-year-old fair-skinned woman has telangiectasias of the cheeks and nose along with red papules and occasional pustules. She also appears to have conjunctivitis with dilated scleral vessels. She reports frequent flushing and blushing. Drinking red wine produces a severe flushing of the face. There is a family history of this condition. Which of the following is the most likely diagnosis?
Carcinoid syndrome
Porphyria cutanea tarda
Lupus vulgaris
Rosacea
Seborrheic dermatitis

98. A 46-year-old construction worker is brought to the clinic by his wife because she has noticed an unusual growth on his left ear for the past 8 months (see photo below). The patient explains that, except for occasional itching, the lesion does not bother him. On physical examination, you notice an 8-mm pearly papule with central ulceration and a few small dilated blood vessels on the border. What is the natural course of this lesion if left untreated?
This is a benign lesion and will not change.
Local invasion of surrounding tissue.
Regression over time
Local invasion of surrounding tissue and metastasis via lymphatic spread.
Disseminated infection resulting in septicemia
99. A 25-year-old postal worker presents with a pruritic, nonpainful skin lesion on the dorsum of his hand. It began like an insect bite but expanded over several days. On examination, the lesion has a black, necrotic center associated with severe local swelling. The patient does not appear to be systemically ill, and vital signs are normal. Which of the following is correct?
The lesion is ecthyma gangrenosum, and blood cultures will be positive for Pseudomonas aeruginosa.
A skin biopsy should be performed and Gram stain examined for gram-positive rods.
The patient has been bitten by Loxosceles reclusa, the brown recluse spider
The patient has the bubo of plague
The patient has necrotizing fasciitis and needs immediate surgical debridemen
100. A 25-year-old who has been living in Washington, DC, presents with a diffuse vesicular rash over his face and trunk. He also has fever. He has no history of chickenpox and has not received the varicella vaccine. Which of the following information obtained from history and physical examination suggests that the patient has chickenpox and not smallpox?
There are vesicular lesions on the palms and soles.
Vesicular lesions are concentrated on the trunk.
The rash is most prominent over the face.
All lesions are at the same stage of development.
The patient experienced high fever several days prior to the rash.
101. A 68-year-old man complains of several blisters arising over the back and trunk for the preceding 2 weeks. He takes no medications and has not noted systemic symptoms such as fever, sore throat, weight loss, or fatigue. The general physical examination is normal. The oral mucosa and the lips are normal. Several 2 to 3 cm bullae are present over the trunk and back. A few excoriations where the blisters have ruptured are present. The remainder of the skin is normal, without erythema or scale. What is the best diagnostic approach at this time?
Culture of vesicular fluid for herpes viruses
Trial of corticosteroids
Biopsy of the edge of a bulla with some surrounding intact skin
CT scan of the chest and abdomen looking for occult malignancy
Combination of oral H1 and H2 antihistamines
102. 63-year-old retired farmer presents to the clinic complaining of red scaly spots on his head for the past 9 months. Physical examination is remarkable for numerous erythematous hyperkeratotic papules and plaques. The lesions are confined to the head and forehead and have poorly defined borders. Which of the following is the most appropriate next step in management of this patient?
Punch biopsy of one of the lesions
Application of hydrocortisone cream to affected areas and follow-up in 4 weeks
Reassurance that this is a benign finding and follow-up in 6 months
Application of fluocinide cream to affected areas and follow-up in 4 weeks
Application of 5-fluorouracil cream to affected areas and follow-up in 4 weeks
103. A 21-year-old female presents with an annular pruritic rash on her neck. She explains that the rash has been present for the past 3 weeks and that her roommate had a similar rash not long ago. Physical examination is remarkable for a 20-mm scaling, erythematous plaque with a serpiginous border. Which of the following is the most appropriate initial treatment for this condition?
A. Griseofulvin
B. Oral cephalexin
C. Topical mupirocin ointment
D. Topical ketoconazole
E. Hydrocortisone cream
104. A 34-year-old homosexual male with a history of HIV presents to the clinic complaining of a wheezing and multiple violaceous plaques and nodules on his trunk and extremities. Physical examination of the oral mucosa reveals similar findings on his palate, gingiva, and tongue. Chest x-ray is also significant for pulmonary infiltrates. What is the most likely pathogenesis of this process?
Proliferation of neoplastic T cells
Infection with human herpesvirus 6
Infection with Mycobacterium avium due to decreasing CD4 count
Angioproliferative disease caused by infection with human herpesvirus 8
Disseminated HSV infection
105. After being fired from his job, a 35-year-old man attempts suicide by drinking from a bottle labeled “insecticide.” Three hours later, emergency medical services (EMS) brings him into the emergency department (ED) and you notice that he is extremely diaphoretic, drooling, and vomiting. He is awake but confused. His vital signs include a blood pressure (BP) of 170/90 mm Hg, heart rate (HR) of 55 beats per minute, respiratory rate (RR) of 22 breaths per minute, temperature of 98.6°F, and oxygen saturation of 95% on room air. Physical examination demonstrates pinpoint pupils and crackles and wheezing on lung examination. What is the treatment to reverse this patient’s poisoning?
Naloxone
N-acetylcysteine (NAC)
Atropine and pralidoxime (2-PAM)
Flumazenil
Physostigmine
106. A 19-year-old man is brought to the ED by EMS after he was found lying on the floor at a dance club. EMS states that the patient seemed unconscious at the dance club, but as soon as they transferred him onto the gurney, he became combative. Upon arrival in the ED, his BP is 120/65 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, RR is 12 breaths per minute, and oxygen saturation is 98% on room air. On physical examination, his pupils are midsized, equal, and reactive to light. His skin is warm and dry. Lung, cardiac, and abdominal examinations are unremarkable. As you walk away from the bedside, you hear the monitor alarm signaling zero respirations and the oxygen saturation starts to drop. You perform a sternal rub and the patient sits up in bed and starts yelling at you. As you leave him for the second time, you hear the monitor alarm again signal zero respirations. You administer naloxone, but there is no change in his condition. Which of the following is most likely the substance ingested by this patient?
γ-Hydroxybutyrate (GHB)
Diazepam
Cocaine
Phencyclidine (PCP)
Heroin
107. A 43-year-old woman presents to the ED with a 3-week history of intermittent headache, nausea, and fatigue. She was seen at her private doctor’s office 1 week ago along with her husband and children, who also have similar symptoms. They were diagnosed with a viral syndrome and told to increase their fluid intake. She states that the symptoms began approximately when it started to get cold outside. The symptoms are worse in the morning and improve while she is at work. Her BP is 123/75 mm Hg, HR is 83 beats per minute, temperature is 98.9°F, and oxygen saturation is 98% on room air. Physical examination is unremarkable. You suspect her first diagnosis was incorrect. Which of the following is the most appropriate next step to confirm your suspicion?
Order a mono spot test
Perform a nasal pharyngeal swab to test for influenza
Consult psychiatry to evaluate for malingering.
Order a carboxyhemoglobin (COHb) level.
Order a lead level.
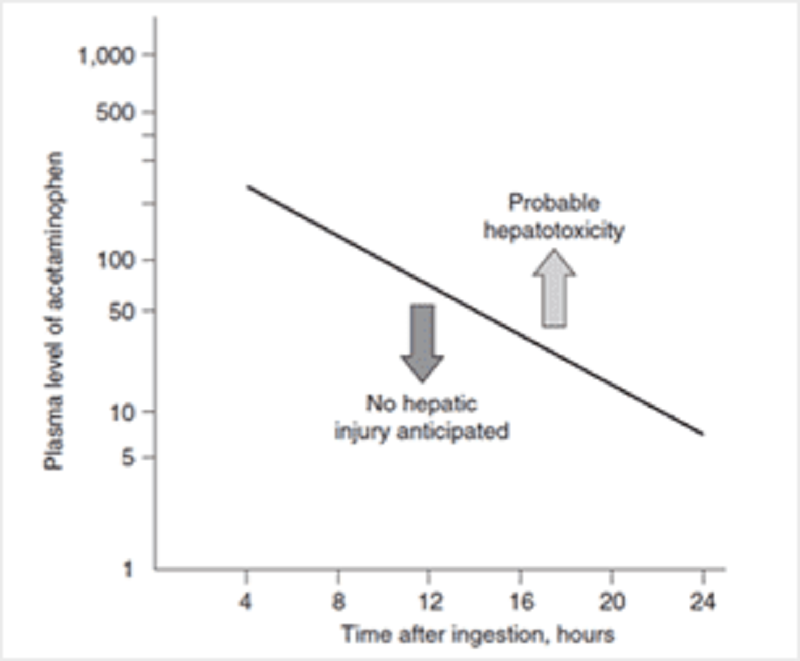
108. An 18-year-old woman is brought to the ED by her mother. The patient is diaphoretic and vomiting. Her mom states that she thinks her daughter tried to commit suicide. The patient admits to ingesting a few handfuls of acetaminophen (Tylenol) approximately 3 hours ago. Her temperature is 99.1 °F, BP is 105/70 mm Hg, HR is 92 beats per minute, RR is 17 breaths per minute, and oxygen saturation is 99% on room air. On examination, her head and neck are unremarkable. Cardiovascular and pulmonary examinations are within normal limits. She is mildly tender in her right upper quadrant, but there is no rebound or guarding. Bowel sounds are normoactive. She is alert and oriented and has no focal deficits on neurologic examination. You administer 50 g of activated charcoal. At this point, she appears well and has no complaints. Her serum acetaminophen (APAP) concentration 4 hours after the reported time of ingestion returns at 350 μg/mL. You plot the level on the nomogram seen below. Which of the following is the most appropriate next step in management?
Discharge home with instructions to return if symptoms return
Observe for 6 hours and, if the patient still has no complaints, discharge her home
Repeat the acetaminophen level 4 hours after the patient arrived in the ED. Treat only if this level is above the line.
Admit to the psychiatry unit and keep on suicide watch while performing serial abdominal examinations
Begin NAC and admit to the hospital
109. A 47-year-old man is brought to the ED by EMS after being found wandering in the street mumbling. His BP is 150/75 mm Hg, HR is 110 beats per minute, temperature is 100.5°F, RR is 16 breaths per minute, oxygen saturation is 99% on room air, and finger stick glucose is 98 mg/dL. On examination, the patient is confused with mumbling speech. His pupils are dilated and face is flushed. His mucous membranes and skin are dry. Which of the following toxic syndromes is this patient exhibiting?
Sympathomimetic syndrome
Anticholinergic syndrome
Cholinergic syndrome
Opioid syndrome
Ethanol syndrome
110. A 25-year-old man is carried into the ED by two of his friends who state that he is not breathing. The patient has a history of heroin abuse. His vital signs are BP 115/70 mm Hg, HR 99 beats per minute, temperature 98.9°F, RR 3 breaths per minute, and oxygen saturation 87% on room air. You notice fresh needle marks and miotic pupils. You begin bag-valve mask ventilation and his oxygen saturation increases to 99%. Which of the following is the most appropriate next step in management?
Continue bag-valve-mask ventilation until he breathes on his own.
Perform endotracheal intubation of the patient
Evaluate response to administration of naloxone
Put the patient on supplemental oxygen
Place a nasogastric tube and administer activated charcoal.
111. A 42-year-old man who is actively seizing is brought to the ED by EMS after a massive ingestion of an unknown substance. The man is known to have a history of acquired immunodeficiency syndrome (AIDS). An intravenous (IV) line is established and anticonvulsant therapy is administered. After high doses of diazepam, phenobarbital, and phenytoin, it is determined that the seizures are refractory to standard anticonvulsant therapy. Which of the following substances did this patient most likely ingest?
Cocaine
Diphenhydramine
Tricyclic antidepressant (TCA)
Haloperidol
Isoniazid (INH)
112. A 60-year-old woman with a history of diabetes is brought into the ED by EMS workers who state that the patient was found on a bus in a lethargic and diaphoretic condition. Her finger stick glucose level at the scene was 35 mg/dL. EMS workers quickly administered dextrose through an IV line. The patient became alert and responsive, stating that she just took her normal medication. Her blood sugar went up to 110 mg/dL and she remained this way throughout her trip to the ED. However, in the ED you notice that the patient is again diaphoretic and is mumbling her speech. Her finger stick glucose is now 47 mg/dL. You administer dextrose and she perks right up. Which of the following diabetes medications commonly causes hypoglycemia for which the patient is likely to require hospital admission?
Regular insulin
Metformin
Glyburide
Sitagliptin
Acarbose
113. A 23-year-old woman presents to the ED complaining of abdominal pain, nausea, and vomiting. She has a history of depression but is not currently taking any antidepressant medications. Upon further questioning, the patient states that she ingested a bottle of pills in her medicine cabinet approximately 3 hours ago. Her BP is 115/65 mm Hg, HR is 101 beats per minute, temperature is 100.1°F, RR is 29 breaths per minute, and oxygen saturation is 100% on room air. Physical examination is unremarkable except for mild diffuse abdominal tenderness. Laboratory results reveal a white blood cell (WBC) count of 10,300/μL, hematocrit 46%, platelets 275/μL, aspartate transaminase (AST) 70 U/L, alanine transaminase (ALT) 85 U/L, alkaline phosphatase 75 U/L, sodium 143 mEq/L, potassium 3.7 mEq/L, chloride 98 mEq/L, bicarbonate 8 mEq/L, blood urea nitrogen (BUN) 22 mg/dL, creatinine 0.9 mg/dL, and glucose 85 mg/dL. Arterial blood gas values on room air are pH 7.51, PCO2 11 mm Hg, and PO2 134 mm Hg. Which of the following substances did this patient most likely ingest?
Diphenhydramine
Ibuprofen
Acetaminophen
Aspirine
Pseudoephedrine
114. A 35-year-old agitated man presents to the ED in police custody. He denies any past medical history and takes no medication. He admits to using some drugs today. His BP is 195/90 mm Hg, HR is 121 beats per minute, temperature is 100.1°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. On examination, he is diaphoretic, and has pupils that are 8 mm in diameter, along with 3+ patella reflexes bilaterally. Electrocardiogram (ECG) reveals sinus tachycardia with a rate of 123. Which of the following toxic syndromes is this patient exhibiting?
Anticholinergic
Cholinergic
Sympathomimetic
Opioid
Sedative hypnotic
115. A 31-year-old woman with a known psychiatric history presents to the ED after ingesting an unknown quantity of pills from her medication vial. In the ED, she complains of nausea, abdominal cramping, and feels unsteady on her feet. On physical examination, you observe that she is tachycardic and ataxic. Which of the following substances will best be treated by activated charcoal that could present like this?
Phenobarbital
Carbamazepine
Lye (sodium hydroxide)
Lithium
Acetaminophen
116. A 27-year-old man presents to the ED extremely agitated complaining of mild chest pain and dyspnea. He states that he was snorting cocaine all afternoon. You place him on a monitor and get his vital signs. His BP is 215/130 mm Hg, HR is 112 beats per minute, temperature is 100.1°F, RR is 17 breaths per minute, and oxygen saturation is 98% on room air. An ECG reveals sinus tachycardia at a rate of 116. Which of the following is the most appropriate medication to administer?
Haloperidol
Labetalol
Esmolol
Diltiazem
Diazepam
117. A 30-year-old man is brought to the ED by police officers. The patient is agitated, vomiting, and complaining of body aches. He states that he is withdrawing from his medication. His vital signs are BP 160/85 mm Hg, RR 20 breaths per minute, HR 107 beats per minute, and temperature 99.7°F. On examination he is diaphoretic, has rhinorrhea, piloerection, and hyperactive bowel sounds. Which of the following substances is this patient most likely withdrawing from?
A. Ethanol
B. Cocaine
C. Nicotine
D. Methadone
E. Clonidine
118. A 25-year-old man is brought into the ED by two police officers because of suspected drug use. The patient is extremely agitated and is fighting the police officers. It takes three hospital staff members and the two police officers to keep him on the stretcher. His vital signs are BP 150/80 mm Hg, HR 107 beats per minute, temperature 99.7°F, RR 18 breaths per minute, and oxygen saturation 99% on room air. Physical examination is unremarkable except for cool, diaphoretic skin, persistent vertical and horizontal nystagmus, and occasional myoclonic jerks. Which of the following is the most likely diagnosis?
Cocaine intoxication
Cocaine withdrawal
Anticholinergic toxidrome
PCP intoxication
Opiate withdrawal
119. An undomiciled 49-year-old man presents to the ED with altered mental status. His BP is 149/75 mm Hg, HR is 93 beats per minute, temperature is 97.5 °F, RR is 18 breaths per minute, and O2 saturation is 99% on room air. Physical examination reveals an unkempt man with the odor of “alcohol” on his breath. His head is atraumatic and pupils are 4 mm, equal, and reactive. The neck is supple. Cardiovascular, pulmonary, and abdominal examinations are unremarkable. There is no extremity edema and his pulses are 2+ and symmetric. Neurologically, he withdraws all four extremities to deep stimuli. ECG is sinus rhythm. Laboratory results reveal: Sodium 141 mEq/L Arterial blood pH 7.26 Potassium 3.5 mEq/L Lactate 1.7 mEq/L Chloride 101 mEq/L Ethanol level undetectable Bicarbonate 14 mEq/L Measured serum osmolarity 352 mOsm/L BUN 15 mg/dL Calculated serum osmolarity 292 mOsm/kg Creatinine 0.7 mg/dL Urinalysis: no blood, ketones, or protein Glucose 89 mg/dL Which of the following statements best describes the laboratory findings?
Anion gap metabolic acidosis and osmol gap
Anion gap metabolic acidosis without osmol gap
Nonanion gap metabolic acidosis and osmol gap
Nonanion gap metabolic acidosis without osmol gap
Metabolic alkalosis with secondary acidosis
120. A 26-year-old woman with a history of depression is brought into the ED. She was found lying on the floor of her apartment next to an unlabeled empty pill bottle. Her HR is 117 beats per minute, BP is 95/65 mm Hg, RR is 14 breaths per minute, and oxygen saturation is 97% on 2-L nasal cannula. On examination, the patient appears obtunded, and her pupils are 3 mm and reactive. Her oropharynx is dry and there is no gag reflex to pharyngeal stimulation. Her neck is supple. The heart is tachycardic without murmurs, the lungs are clear to auscultation, and the abdomen is soft. There is normal rectal tone and brown stool that is heme negative. Her skin is cool and moist with no signs of needle tracks. Neurologically, she is unresponsive but withdraws all extremities to deep palpation. Finger stick blood glucose is 85 mg/dL. Her ECG reveals sinus tachycardia at 119 with a QRS complex of 140 milliseconds and a terminal R wave in lead aVR. Which of the following is the most appropriate next step in management?
Orotracheal intubation, administer activated charcoal through orogastric tube, and IV naloxone
Orotracheal intubation, administer activated charcoal through orogastric tube, and IV sodium bicarbonate
Orotracheal intubation, administer activated charcoal through orogastric tube, and IV NAC
Orotracheal intubation, administer syrup of ipecac through orogastric tube, and IV sodium bicarbonate
Induce vomiting prior to intubation to lower the risk of aspiration then administer IV sodium bicarbonate
121. A 37-year-old woman is brought into the ED by her friend who states that the patient swallowed approximately 50 capsules of 325-mg acetaminophen (APAP) 6 hours ago in an attempted suicide. The patient states she feels nauseated and vomits while you take her history. Her BP is 100/75 mm Hg, HR is 97 beats per minute, temperature is 98.9°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. Examination is unremarkable except for mild epigastric tenderness. Which of the following is the correct antidote for APAP overdose?
NAC
Physostigmine
Flumazenil
Naloxone
Digibind
122. A 31-year-old man is brought to the ED by EMS who state that the man was found lying on the floor of his garage. He is rousable in the ED, speaks with slurred speech, and vomits. His BP is 140/85 mm Hg, HR is 94 beats per minute, temperature is 98.8°F, RR is 17 breaths per minute, and oxygen saturation is 99% on room air. You place an IV line, draw blood, and start a liter of normal saline running through the line. Laboratory results reveal serum sodium 139 mEq/L, potassium 3.5 mEq/L, chloride 101 mEq/L, bicarbonate 14 mEq/L, BUN 15 mg/dL, creatinine 1 mg/dL, glucose 105 mg/dL, arterial blood pH 7.27, COHb 4%, and lactate 2.8 mEq/L. Urinalysis shows 1+ protein, trace ketones, WBC 4/hpf (high-power field), red blood cell (RBC) 2 to 3/hpf, and multiple envelope-shaped and needleshaped crystals. Which of the following conditions would best explain his metabolic acidosis?
Ibuprofen toxicity
Ethylene glycol poisoning
Diabetic ketoacidosis (DKA)
Lactic acidosis
Isopropyl alcohol poisoning
E. Isopropyl alcohol poisoning 123. A 35-year-old man who is employed as a forklift operator was found sitting outside a warehouse. He came stumbling out complaining of dizziness and headaches. Coworkers in an adjoining warehouse also complained of headache and nausea. After collapsing outside, he regained consciousness immediately but appeared confused. In the ED, his BP is 100/54 mm Hg, HR is 103 beats per minute, temperature is 100°F, pulse ox is 91% on room air, and RR is 23 breaths per minute. Physical examination is unremarkable. Laboratory results reveal WBC 10,500/μL, hematocrit 45%, platelets 110/μL, sodium 137 mEq/L, potassium 4 mEq/L, chloride 103 mEq/L, bicarbonate 21 mEq/L, BUN 8 mg/dL, creatinine 0.5 mg/dL, and glucose 89 mg/dL. Arterial blood gas results are pH 7.32, PCO2 32 mm Hg, and PO2 124 mm Hg. Which of the following is the most likely diagnosis?
Methemoglobinemia
Hypoglycemic syncope
Hydrocarbon poisoning
Opioid overdose
CO poisoning
124. A 51-year-old man presents to the ED complaining of nausea and abdominal pain after drinking some “bitter stuff.” He is considered one of the “regulars” who is usually at triage with ethanol intoxication. His temperature is 97.9°F, BP is 130/65 mm Hg, HR is 90 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 97% on room air. Physical examination is unremarkable, except for slurred speech and the smell of acetone on the patient’s breath. Laboratory results reveal serum sodium 138 mEq/L, potassium 3.5 mEq/L, chloride 105 mEq/L, bicarbonate 23 mEq/L, BUN 10 mg/dL, creatinine 2.1 mg/dL, glucose 85 mg/dL, arterial blood pH 7.37, and lactate 1.4 mEq/L. Urinalysis shows moderate ketones. Which of the following is the most likely diagnosis?
DKA
Ethanol intoxication
Methanol intoxication
Isopropyl alcohol intoxication
Ethylene glycol intoxication
125. A 55-year-old man presents to the ED 6 hours after ingesting two bottles of his baby aspirin. He complains of nausea, vomiting, dizziness, and tinnitus. His temperature is 100.3°F, BP is 140/80 mm Hg, HR is 105 beats per minute, RR is 31 breaths per minute, and oxygen saturation is 99% on room air. Arterial blood gas on room air reveals a pH of 7.52, PCO2 10 mm Hg, and PO2 129 mm Hg. The blood salicylate level returns at 45 mg/dL. Which of the following is the most appropriate next step in management?
Administer activated charcoal, begin IV hydration, and administer sodium bicarbonate
Administer activated charcoal, begin IV hydration, and intubate the patient for respiratory failure.
Administer activated charcoal, begin IV hydration, and administer NAC
Arrange for immediate hemodialysis
Gastric lavage, IV hydration, and repeat levels before beginning therapy.
126. A 40-year-old man with a known history of ethanol abuse states that 2 hours ago he ingested two bottles of extrastrength Tylenol. The patient has no medical complaints except for some nausea. At 4 hours postingestion, you send blood to the laboratory to measure the serum acetaminophen concentration. The level returns and falls above the treatment line when you plot it on the APAP nomogram. You administer activated charcoal and decide to start IV NAC. Which of the following is a known adverse effect of IV NAC administration?
Hepatic failure
Anaphylactoid reaction
Hypertensive crisis
Confusion
Change in urine color
127. A 19-year-old woman presents to the ED with abdominal pain, nausea, vomiting, diarrhea, and hematemesis after ingesting an unknown substance in a suicide attempt. Which of the following antidotes are correctly paired?
Organophosphate—Physostigmine
Iron overdose—Deferoxamine
Aspirin overdose—NAC
Acetaminophen overdose—Naloxone
Anticholinergic overdose—Fomepizole
128. A 34-year-old woman presents to the ED after ingesting an unknown quantity of her antidepressant pills. EMS workers found an empty bottle of amitriptyline on her apartment floor. She is awake but appears delirious. Her BP is 130/65 mm Hg, HR is 101 beats per minute, temperature is 99.1°F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. On examination, her pupils are 7 mm and reactive. Her face is flushed and mucous membranes are dry. Her lungs are clear and heart is without murmurs. The abdomen is soft, nontender, and with decreased bowel sounds. She is moving all four extremities. ECG reveals sinus rhythm at a rate of 99 and QRS just under 100 milliseconds. In a TCA overdose, which of the following is responsible for her mydriasis, dry mucous membranes, and delirium?
Sodium channel blockade
Muscarinic receptor blockade
Inhibition of serotonin and norepinephrine reuptake
Histamine receptor blockade
α-Receptor blockade
129. You receive notification from EMS that they are bringing in a 17-yearold adolescent boy who was found unconscious by a police officer. The police officer at the scene states that he snuck up on a group of kids that he thought were using drugs. Two of them got away and one just fell to the ground seconds after standing up. Lying on the ground next to the adolescent were plastic bags. The emergency medical technician (EMT) states that the patient was in ventricular fibrillation. He was shocked in the field and is now in a sinus rhythm. The EMT also administered IV dextrose, thiamine, and naloxone without any change in mental status. Which of the following substances was the patient most likely abusing?
Butane
Ethanol
Heroin
Cocaine
PCP
130. A 61-year-old man with a history of depression and hypertension is brought to the ED by EMS for altered mental status. The patient’s wife states that he stopped taking his fluoxetine 1 month ago and now only takes metoprolol for his hypertension. The patient’s BP is 75/40 mm Hg, HR is 39 beats per minute, RR is 14 breaths per minute, oxygen saturation is 99% on 100% oxygen, and fingerstick glucose is 61 mg/dL. The patient is awake and moaning, responding only to deep stimuli. His extremities are cool to the touch. You suspect an overdose of metoprolol. You endotracheally intubate the patient for airway control. Which of the following is the most appropriate next step in management?
Normal saline bolus, administer atropine, administer 1-g calcium gluconate bolus, then insert a transvenous cardiac pacer
Put the patient on pacer pads, then administer norepinephrine drip
Cardioversion with 200 J, then administer atropine
Normal saline bolus, atropine, norepinephrine
Normal saline bolus, atropine, glucagon
131. A 22-year-old woman presents to the ED by ambulance from a dance club. The paramedics report that the patient was agitated in the club and had a generalized seizure. Her BP is 165/100 mm Hg, HR is 119 beats per minute, temperature is 101.9 °F, RR is 17 breaths per minute, oxygen saturation is 98% on room air, and fingerstick glucose is 92 mg/dL. On examination, the patient is hyperactive and appears to be hallucinating. Her pupils are dilated to 6 mm bilaterally and reactive. Her neck is supple. Examination of the heart is unremarkable except for tachycardia. Her lungs are clear and abdomen is soft and nontender. The patient moves all four extremities. Laboratory results are as follows: Sodium 109 mEq/L WBC 12,000/mm 3 Potassium 3.5 mEq/L Hct 49% Chloride 83 mEq/L Platelets 350/μL Bicarbonate 20 mEq/L BUN 10 mg/dL Creatinine 1 mg/dL Glucose 103 mg/dL Which of the following substances did this patient most likely consume?
Cocaine
Heroin
3,4-Methylenedioxymethamphetamine (MDMA)
Ketamine (special K)
PCP
132. An asymptomatic young adult was brought to the ED by a police officer after his home was raided. The patient swallowed five small packets of an unknown substance before being arrested. His BP is 125/75 mm Hg, HR is 85 beats per minute, temperature is 98.7°F, and RR is 16 breaths per minute. Physical examination is unremarkable. An abdominal radiograph confirms intraluminal small bowel densities. Which of the following is the most appropriate treatment?
Magnesium citrate
Gastric lavage
Activated charcoal and polyethylene glycol
Syrup of ipecac
NAC
133. A 33-year-old woman presents to the ED with a painful sprained ankle. She has a past medical history of depression for which she is taking phenelzine, a monoamine oxidase inhibitor. After you place an elastic wrap on her ankle, she asks you to prescribe her some pain medication. Which of the following medications is contraindicated in patients taking a monoamine oxidase inhibitor?
Ibuprofen
Acetaminophen
Meperidine
Oxycodone
Hydrocodone
134. A 27-year-old woman presents to the ED 6 hours after the onset of body aches, abdominal cramping, and diarrhea. She is currently visiting relatives and normally lives in another state. She regularly takes six to eight tablets daily of hydrocodone for chronic low-back pain, sumatriptan for migraines, and amitriptyline and paroxetine for bulimia nervosa. Her BP is 130/80 mm Hg, HR is 100 beats per minute, temperature is 98.6°F, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. Examination shows diaphoresis, dilated pupils, and piloerection. Neurologically she is moving all four extremities and you do not note tremors. She is alert and cooperative but seems restless. She denies hallucinations or suicidal ideations. She becomes very angry when you ask her for the phone numbers of her regular physicians. Which of the following is the most likely explanation of her symptoms?
Anticholinergic overdose
TCA intoxication
Ethanol withdrawal
Serotonin syndrome
Opiate withdrawal
135. A 58-year-old woman is brought to the emergency department (ED) by emergency medical service (EMS) after slipping on a patch of ice while walking to work and hitting her head on the cement pavement. Bystanders acknowledged that the patient was unconscious for approximately 1 minute. On arrival, her vital signs are blood pressure (BP) 155/75 mm Hg, heart rate (HR) 89 beats per minute, respiratory rate (RR) 18 breaths per minute, and pulse oxygenation 98% on room air. She has a 5-cm laceration to the back of her head that is actively bleeding. You ask the patient what happened but she cannot remember. You inform her that she is in the hospital as a result of a fall. Over the next 10 minutes she asks you repeatedly what happened and where she is. You do not find any focal neurologic deficits. As you bring the patient to the CT scanner, she vomits once. CT results show a normal brain scan. Which of the following is the most likely diagnosis?
Cerebral concussion
Diffuse axonal injury
Cerebral contusion
Posttraumatic epilepsy
Trauma-induced Alzheimer disease
136. A 41-year-old man, the restrained driver in a high-speed motor vehicle collision, is brought to the ED by EMS. The patient is breathing without difficulty with bilateral and equal breaths sounds. He has strong pulses peripherally indicating a BP of at least 90 mm Hg. The HR is 121 beats per minute. His Glasgow coma scale (GCS) is 14. A secondary survey reveals chest wall bruising. You suspect a cardiac injury. Which of the following locations most commonly involve cardiac contusions?
Right atrium
Right ventricle
Left atrium
Left ventricle
Septum
137. A 25-year-old man is brought into the trauma resuscitation room after his motorcycle is struck by another vehicle. EMS reports that the patient was found 20 ft away from his motorcycle, which was badly damaged. His vital signs include a BP of 90/60 mm Hg, HR 115 beats per minute, RR 22 breaths per minute, and pulse oxygenation of 100% on facemask. Which of the following is the smallest amount of blood loss that produces a decrease in the systolic BP in adults
Loss of 5% of blood volume
Loss of 10% of blood volume
Loss of 15% to 30% of blood volume
Loss of 30% to 40% of blood volume
Loss of greater than 40% of blood volume
138. You are notified by the EMS dispatcher that there is a multiple-car collision on the local highway with many injuries. He states that there are two people dead at the scene, one person is critically injured and hypotensive, and three people have significant injuries but with stable vital signs. Which of the following is the leading cause of death and disability in trauma victims?
Abdominal injury
Thoracic injury
Back injury
Cervical injury
Head injury
139. Paramedics bring a 17-year-old high school football player to the ED on a backboard and with a cervical collar. During a football game, the patient “speared” another player with his helmet and subsequently experienced severe neck pain. He denies paresthesias and is able to move all of his extremities. A cervical spine CT scan reveals multiple fractures of the first cervical vertebra. Which of the following best describes this fracture?
Odontoid fracture
Hangman’s fracture
Jefferson fracture
Clay shoveler’s fracture
Teardrop fracture
140. A 20-year-old man presents to the ED with multiple stab wounds to his chest. His BP is 85/50 mm Hg and HR is 123 beats per minute. Two large-bore IVs (intravenous) are established and running wide open. On examination, the patient is mumbling incomprehensibly, has good air entry on lung examination, and you notice jugular venous distension (JVD). As you are listening to his heart, the nurse calls out that the patient has lost his pulse and that she cannot get a BP reading. Which of the following is the most appropriate next step in management?
Atropine
Epinephrine
Bilateral chest tubes
ED thoracotomy
Pericardiocentesis
141. A 22-year-old man calls the ED from a local bar stating that he was punched in the face 10 minutes ago and is holding his front incisor tooth in his hand. He wants to know what the best way is to preserve the tooth. Which of the following is the most appropriate advice to give the caller?
Place the tooth in a napkin and bring it to the ED.
Place the tooth in a glass of water and bring it to the ED.
Place the tooth in a glass of beer and bring it to the ED.
Pour some water over the tooth and place it immediately back into the socket.
Place the tooth in a glass of milk and bring it to the ED.
142. A 19-year-old man is brought into the trauma room by EMS after a head-on cycling accident. The patient was not wearing a helmet. Upon presentation his BP is 125/75 mm Hg, HR is 105 beats per minute, RR is 19 breaths per minute, and oxygen saturation is 100% on mask. His eyes are closed but open to command. He can move his arms and legs on command. When you ask him questions, he is disoriented but able to converse. What is this patient’s GCS score?
11
12
14
13
15
143. An 18-year-old man presents to the ED after getting stabbed in his abdomen. His HR is 140 beats per minute and BP is 90/40 mm Hg. He is yelling that he is in pain. Two large-bore IVs are inserted into his antecubital fossa and fluids are running wide open. After 2 L of fluids, his BP does not improve. Which of the following is the most common organ injured in stab wounds?
Liver
Small bowel
Stomach
Colon
Spleen
144. A 61-year-old man presents to the ED with chest wall pain after a motor vehicle collision. He is speaking full sentences, breath sounds are equal bilaterally, and his extremities are well-perfused. His BP is 150/75 mm Hg, HR is 92 beats per minute, and oxygen saturation is 97% on room air. Chest radiography reveals fractures of the seventh and eighth ribs of the right anterolateral chest. He has no other identifiable injuries. Which of the following is the most appropriate treatment for this patient’s rib fractures?
Apply adhesive tape on the chest wall perpendicular to the rib fractures.
Insert a chest tube into the right thorax.
Bring the patient to the OR for surgical fixation
Analgesia and incentive spirometry
Observation.
E. Observation. 145. A 27-year-old man brought to the ED by paramedics after a motor vehicle collision. His RR is 45 breaths per minute, oxygen saturation is 89%, HR is 112 beats per minute, and BP is 115/75 mm Hg. You auscultate his chest and hear decreased breath sounds on the left. Which of the following is the most appropriate next step in management?
Order a stat chest radiograph
Perform a pericardiocentesis
Perform a diagnostic peritoneal lavage (DPL).
Perform an ED thoracotomy.
Perform a tube thoracostomy
146. A 29-year-old man is brought to the ED by EMS after being stabbed in the left side of his back. His BP is 120/80 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 98% on room air. On the secondary survey, you note motor weakness of his left lower extremity and the loss of pain sensation in the right lower extremity. Which of the following is the most likely diagnosis?
Spinal shock
Central cord syndrome
Anterior cord syndrome
Brown-Sequard syndrome
Cauda equina syndrome
147. A 33-year-old man, who was drinking heavily at a bar, presents to the ED after getting into a fight. A bystander tells paramedics that the patient was punched and kicked multiple times and sustained multiple blows to his head with a stool. In the ED, his BP is 150/75 mm Hg, HR is 90 beats per minute, RR is 13 breaths per minute, and oxygen saturation is 100% on non-rebreather. On examination, he opens his eyes to pain and his pupils are equal and reactive. There is a laceration on the right side of his head. He withdraws his arm to pain but otherwise does not move. You ask him questions, but he just moans. Which of the following is the most appropriate next step in management?
Prepare for intubation
Suture repair of head laceration.
Administer mannitol
Bilateral burr holes
Neurosurgical intervention
148. A 74-year-old man presents to the ED after being involved in a motor vehicle collision. He states he was wearing his seat belt in the driver’s seat when a car hit him from behind. He thinks his chest hit the steering wheel and now complains of pain with breathing. His RR is 20 breaths per minute, oxygen saturation is 98% on room air, BP is 145/75 mm Hg, and HR is 90 beats per minute. On examination, you notice paradoxical respirations. Which of the following best describes a flail chest?
One rib with three fracture sites
Two adjacent ribs, each with two fracture sites
Three adjacent ribs, each with two fracture sites
One fractured right-sided rib and one fractured left-sided rib
Two fractured right-sided ribs and two fractured left-sided ribs
149. A 29-year-old man presents to the ED after being stabbed in his neck. The patient is speaking in full sentences. His breath sounds are equal bilaterally. His BP is 130/75 mm Hg, HR is 95 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. The stab wound is located between the angle of the mandible and the cricoid cartilage and violates the platysma. There is blood oozing from the site although there is no expanding hematoma. Which of the following is the most appropriate next step in management?
Explore the wound and blind clamp any bleeding site.
Probe the wound looking for injured vessels.
Apply direct pressure and bring the patient immediately to the OR to explore the zone I injury.
Apply direct pressure and bring the patient immediately to the OR to explore the zone II injury.
Apply direct pressure and bring the patient immediately to the OR to explore the zone III injury.
150. A 45-year-old man is brought to the ED after a head-on motor vehicle collision. Paramedics at the scene tell you that the front end of the car is smashed. The patient’s BP is 130/80 mm Hg, HR is 100 beats per minute, RR is 15 breaths per minute, and oxygen saturation is 98% on room air. Radiographs of the cervical spine reveal bilateral fractures of the C2 vertebra. The patient’s neurologic examination is unremarkable. Which of the following best describes this fracture?
Colles fracture
Boxer’s fracture
Jefferson fracture
Hangman’s fracture
Clay shoveler’s fracture
151. A 71-year-old man is found lying on the ground one story below the balcony of his apartment. Paramedics bring the patient into the ED. He is cool to touch with a core body temperature of 96°F. His HR is 119 beats per minute and BP is 90/70 mm Hg. His eyes are closed, but they open when you call his name. His limbs move to stimuli, and he answers your questions but is confused. On examination, you note clear fluid dripping from his left ear canal and an area of ecchymosis around the mastoid bone. Which of the following is the most likely diagnosis?
Le Fort fracture
Basilar skull fracture
Otitis interna
Otitis externa
Tripod fracture
152. A 34-year-old construction worker is brought to the ED by EMS after falling 30 ft from a scaffold. His vital signs are HR 124 beats per minute, BP 80/40 mm Hg, and oxygen saturation 93% on 100% oxygen. He has obvious head trauma with a scalp laceration overlying a skull fracture on his occiput. He does not speak when asked his name, his respirations are poor, and you hear gurgling with each attempted breath. Auscultation of the chest reveals diminished breath sounds on the right. There is no JVD or anterior chest wall crepitus. His pelvis is unstable with movement laterally to medially and you note blood at the urethral meatus. His right leg is grossly deformed at the knee and there is an obvious fracture of his left arm. Which of the following is the most appropriate next step in management?
Insert a 32F chest tube into the right thoracic cavity.
Perform a DPL to rule out intra-abdominal hemorrhage
Create two Burr holes into the cranial vault to treat a potential epidural hematoma
Immediately reduce the extremity injuries and place in a splint until the patient is stabilized.
Plan for endotracheal intubation of the airway with in-line stabilization of the cervical spine.
153. A 20-year-old man was found on the ground next to his car after it hit a tree on the side of the road. Bystanders state that the man got out of his car after the collision but collapsed within a few minutes. Paramedics subsequently found the man unconscious on the side of the road. In the ED, his BP is 175/90 mm Hg, HR is 65 beats per minute, temperature is 99.2°F, RR is 12 breaths per minute, and oxygen saturation is 97% on room air. Physical examination reveals a right-sided fixed and dilated pupil. A head CT is shown below. Which of the following is the most likely diagnosis?
Epidural hematoma
Subdural hematoma
Subarachnoid hemorrhage (SAH)
Intracerebral hematoma
Cerebral contusion
154. An 81-year-old woman presents to the ED after tripping over the sidewalk curb and landing on her chin causing a hyperextension of her neck. She was placed in a cervical collar by paramedics. On examination, she has no sensorimotor function of her upper extremities. She cannot wiggle her toes, has 1/5 motor function of her quadriceps, and only patchy lower extremity sensation. Rectal examination reveals decreased rectal tone. Which of the following is the most likely diagnosis?
Central cord syndrome
Anterior cord syndrome
Brown-Sequard syndrome
Transverse myelitis
Exacerbation of Parkinson disease
155. A 22-year-old man presents to the ED after being ejected from his vehicle following a high-speed motor vehicle collision. Upon arrival, his BP is 85/55 mm Hg and HR is 141 beats per minute. Two large-bore IVs are placed in the antecubital veins and lactated Ringer solution is being administered. After 3 L of crystalloid fluid, the patient’s BP is 83/57 mm Hg. Which of the following statements is most appropriate regarding management of a hypotensive trauma patient who fails to respond to initial volume resuscitation? a. It is important to wait for fully cross-matched blood
It is important to wait for fully cross-matched blood prior to transfusion.
Whole blood should be used rather than packed red blood cells (RBCs).
Blood transfusion should begin after 4 L of crystalloid infusion.
Type O blood that is Rh-negative should be transfused.
Type O blood that is Rh-positive should be transfused
156. A 24-year-old man is brought into the ED by paramedics after being run over by a car. His systolic BP is 90 mm Hg by palpation, HR is 121 beats per minute, RR is 28 breaths per minute, and oxygen saturation is 100% on non-rebreather. The airway is patent and breath sounds are equal bilaterally. You establish large-bore access and fluids are running wide open. Secondary survey reveals an unstable pelvis upon movement with lateral to medial force. Bedside focused abdominal sonography for trauma (FAST) is negative for intraperitoneal fluid. Which of the following is the most appropriate immediate next step in management?
Bilateral chest tubes
Application of external fixator
Application of pelvic binding apparatus
Venographic embolization
Angiographic embolization
157. A 32-year-old man is brought to the ED by paramedics after a diving accident. The lifeguard on duty accompanies the patient and states that he dove head first into the shallow end of the pool and did not resurface. On examination, the patient is speaking but cannot move his arms or legs and cannot feel pain below his clavicle. He is able to feel light touch and position of his four extremities. A cervical spine radiograph does not reveal a fracture. Which of the following is the most likely diagnosis?
Spinal cord injury without radiographic abnormality (SCIWORA)
Central cord syndrome
Anterior cord syndrome
Cauda equina syndrome
Brown-Sequard syndrome
158. A 22-year-old man is brought to the ED 20 minutes after a head-on motor vehicle collision in which he was the unrestrained driver. On arrival, he is alert and coherent but appears short of breath. His HR is 117 beats per minute, BP is 80/60 mm Hg, and oxygen saturation is 97% on a nonrebreather. Examination reveals bruising over the central portion of his chest. His neck veins are not distended. Breath sounds are present on the left but absent on the right. Following administration of 2 L of lactated Ringer solution, his systolic BP remains at 80 mm Hg. Which of the following is the most appropriate next step in management?
Sedate, paralyze, and intubate.
Perform a needle thoracostomy
Perform a DPL.
Perform a FAST examination.
Perform a pericardiocentesis
159. An 87-year-old man is brought to the ED on a long board and in a cervical collar after falling down a flight of steps. He denies losing consciousness. On arrival, his vital signs include an HR of 99 beats per minute, BP of 160/90 mm Hg, and RR of 16 breaths per minute. He is alert and speaking in full sentences. Breath sounds are equal bilaterally. Despite an obvious right arm fracture, his radial pulses are 2+ and symmetric. When examining his cervical spine, he denies tenderness to palpation and you do not feel any bony deformities. Which of the following is a true statement?
Epidural hematomas are very common in the elderly age population.
Cerebral atrophy in the elderly population provides protection against subdural hematomas.
Increased elasticity of their lungs allows elderly patients to recover from thoracic trauma more quickly than younger patients.
The most common cervical spine fracture in this age group is a wedge fracture of the sixth cervical vertebra.
Despite lack of cervical spine tenderness, imaging of his cervical spine is warranted
160. A 45-year-old man is brought into the ED after a head-on motor vehicle collision. His BP is 85/45 mm Hg and HR is 130 beats per minute. He is speaking coherently. His breath sounds are equal bilaterally. After 2 L of fluid resuscitation, his BP is 80/40 mm Hg. A FAST examination reveals fluid in Morison pouch. Which of the following organs is most likely to be injured in blunt abdominal trauma?
Liver
Spleen
Kidney
Small bowel
Bladder
161. A 47-year-old man is brought into the ED after falling 20 ft from a ladder. His HR is 110 beats per minute, BP is 110/80 mm Hg, RR is 20 breaths per minute, and oxygen saturation is 100% on face mask. He is able to answer your questions without difficulty. His chest is clear with bilateral breath sounds, abdomen is nontender, pelvis is stable, and the FAST examination is negative. You note a large scrotal hematoma and blood at the urethral meatus. Which of the following is the most appropriate next step in management?
Scrotal ultrasound
Kidney-ureter-bladder (KUB) radiograph
IV pyelogram
Retrograde cystogram
Retrograde urethrogram
162. A 17-year-old man presents to the ED after getting hit in the right eye with a tennis ball during a tennis match. On arrival to the ED, you note periorbital swelling and ecchymosis. The patient’s visual acuity is 20/20. When you are testing his extraocular muscles, you note that his right eye cannot look superiorly but his left eye can. He also describes pain in his right eye when attempting to look upward. Which of the following is the most likely diagnosis?
Zygomatic arch fracture
Orbital floor fracture
Retrobulbar hematoma
Ruptured globe
Mandible fracture with entrapment of the pterygoid
163. A 24-year-old man is brought to the ED after being shot once in the abdomen. On arrival, his BP is 100/60 mm Hg, HR is 115 beats per minute, and RR is 22 breaths per minute. His airway is patent and you hear breath sounds bilaterally. On abdominal examination, you note a single bullet entry wound approximately 1 cm to the right of the umbilicus. During the log roll, you see a single bullet exit wound approximately 3 cm to the right of the lumbar spine. His GCS score is 15. The patient’s BP is now 85/65 mmHg and HR is 125 beats per minute after 2L of fluid. Which of the following is the most appropriate next step in management?
Probe the entry wound to see if it violates the peritoneum
Perform a FAST examination
Perform a DPL
Take the patient directly to the CT scanner.
Take the patient directly to the OR
164. A 43-year-old man, who currently uses drugs intravenously (IV), presents to the emergency department (ED) with 2 weeks of fever, back pain, and progressive weakness in his legs bilaterally. He denies any history of trauma or prior surgery. His blood pressure (BP) is 130/75 mm Hg, heart rate (HR) is 106 beats per minute, temperature is 103°F, and respiratory rate (RR) is 16 breaths per minute. On physical examination, he has tenderness to palpation in the mid-lumbar spine, increased patellar reflexes, and decreased strength in the lower extremities bilaterally, with normal range of motion. Laboratory results reveal a white blood cell (WBC) count of 15,500/μL, hematocrit 40%, and platelets 225/μL. Urinalysis and spinal x-rays are unremarkable. Which of the following is the most likely diagnosis?
Fibromyalgia
Ankylosing spondylitis
Spinal epidural abscess
Vertebral compression fracture
Spinal metastatic lesion
165. An 81-year-old woman is brought to the ED by her children who state that the patient is acting more tired than usual, has had fever for the last 2 days, and is more confused. Ordinarily, the patient is high functioning: she is ambulatory, cooks for herself, and walks on a treadmill 30 minutes a day. Her vital signs are BP 85/60 mm Hg, HR 125, RR 20, temperature 101.3°F, and pulse oxygenation 97% on room air. On examination, the patient has dry mucous membranes but is otherwise unremarkable. She is oriented to person and place but states that the year is 1925. Her laboratory results show a WBC 14,300/μL, hematocrit 31%, and platelets 350/μL. Her electrolytes are within normal limits. Blood glucose is 92 mg/dL. A chest radiograph does not show any infiltrates. Urinalysis reveals 2+ protein, trace ketones, WBC > 100/hpf, red blood cell (RBC) 5 to 10/hpf, nitrite positive, and leukocyte esterase positive. After administering a 500-cc normal saline fluid bolus and broad-spectrum antibiotics through her peripheral IV line, the patient’s BP is 82/60 mm Hg. You suspect that the patient is in septic shock due to an acute urinary tract infection. Which of the following is the next most appropriate course of action to manage this patient with earlygoal-directed therapy (EGDT)?
Immediately start a norepinephrine infusion to increase the blood pressure given the low systolic blood pressure.
Prepare to transfuse uncrossed matched packed RBC to increase oxygen-carrying capacity given the low hematocrit.
Place a central venous line into the right internal jugular vein to measure central venous pressure (CVP).
Transport the patient to radiology for a stat CT scan of her head given the acute change in mental status.
Place a central venous line into the right internal jugular vein to measure mixed venous oxygen saturation (SVO2).
166. A 23-year-old man presents to the ED with left lower abdominal pain and left testicular pain that started 1 to 2 weeks ago and has gradually worsened. He has some nausea and vomiting. His HR is 98 beats per minute, BP is 125/65 mm Hg, temperature is 100.9°F, and RR is 18 breaths per minute. Physical examination reveals a tender left testicle with a firm nodularity on the posterolateral aspect of the testicle. Pain is relieved slightly with elevation of the testicle and the cremasteric reflex in normal. You make the presumptive diagnosis of epididymitis. Which of the following is the next best step?
Prescribe pain medications and penicillin for coverage of syphilis, the most likely causative organism.
Recommend bed rest, ice, and scrotal elevation with prompt urology follow-up.
Give ceftriaxone 125 mg intramuscularly (IM), plus a one-time dose of azithromycin 1g orally
Give ceftriaxone 250 mg intramuscularly (IM), plus a 10-day course of oral doxycycline.
Confirm the diagnosis with transillumination of the testicle, and then consult urology for surgical drainage
167. A 40-year-old man with insulin-dependent diabetes presents to the ED with complaints of 2 days of increasingly severe perineal pain and subjective fevers. His HR is 118 beats per minute, BP is 95/55 mm Hg, temperature is 103.4°F, and RR is 22 breaths per minute. The bedside sugar reading is “high.” Physical examination demonstrates crepitus over the medial thigh and widespread erythema and purple discoloration with sharp demarcation over the scrotum. The scrotum is markedly tender, warm, and edematous. Which of the following is the most likely diagnosis?
Cutaneous candidiasis
Fournier syndrome
Phimosis
Paraphimosis
Testicular torsion
168. A 55-year-old man with a history of diabetes presents with complaints of developed left knee pain several days following a fall from standing height. The patient was brought to the ED by ambulance after being found on a park bench stating he was unable to walk because of the pain. On physical examination, there are no rashes or external signs of trauma. His left knee is warm, diffusely tender, and swollen with a large effusion. He has pain on passive range of motion and is refusing to walk. His BP is 150/85 mm Hg, HR is 105 beats per minute, temperature is 102.7°F, RR is 16 breaths per minute, and fingerstick glucose is 89 mg/dL. Which of the following is the most appropriate diagnostic test?
Knee radiographs
Magnetic resonance imaging (MRI)
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
Arthrocentesis
Bone scan
169. A 35-year-old woman with systemic lupus erythematosus (SLE) is brought to the ED by her brother after he found her febrile and confused. Physical examination reveals fever, tachycardia, a waxing and waning mental status, petechiae over her oral mucosa, pallor, and mildly heme-positive stool. Her urinalysis is positive for blood, red cell casts, and proteinuria. Laboratory results reveal blood urea nitrogen (BUN) of 40 mg/dL and creatinine of 2 mg/dL. Her bilirubin is elevated (unconjugated > conjugated) and her international normalized ratio (INR) is 0.98. Her complete blood count reveals WBC 12,000/μL, hematocrit 29%, and platelet count 17,000/μL with schistocytes on the peripheral smear. Which of the following is the most appropriate next step in management?
Admit to the intensive care unit (ICU) for plasmapheresis and close monitoring for acute bleeds.
Admit to the ICU for platelet transfusion and monitoring for acute bleeds.
Admit to the ICU for corticosteroid infusion, transfusion of platelets, and prompt surgical consultation for emergent splenectomy.
Admit to the ICU for dialysis and close monitoring for acute bleeds.
Perform a noncontrast head computed tomography (CT) to screen for intracranial bleeding and mass effect followed by a lumbar puncture (LP) for analysis of cerebrospinal fluid (CSF). If negative, admit to telemetry for hemodynamic monitoring.
171. A 32-year-old diabetic man presents to the ED with a fever and 1 week of increasing right foot pain. He states he stepped on a nail while running barefoot 2 weeks ago but didn’t think much of it at that time. On physical examination, his heel is mildly erythematous and diffusely tender to palpation, with overlying warmth and edema. There is a small amount of purulent drainage through the puncture hole in his heel. A plain radiograph of his foot demonstrates a slight lucency of the calcaneus. He has decreased range of motion, but you are able to passively dorsiflex and plantarflex his ankle without difficulty. His vital signs include a temperature of 101.4°F, HR of 98 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. Which of the following is the most common causative organism of this condition?
Salmonella sp
Pseudomonas aeruginosa
Staphylococcus aureus
Group B streptococci
Pasteurella multocida
172. A 75-year-old woman is transferred to your ED from the local nursing home for fever, cough, and increasing lethargy. Over the past 3 days, the nursing home staff noticed increasing yellow sputum and decreasing urine output from the patient. Her BP is 118/75 mm Hg, RR is 20 breaths per minute, HR is 105 beats per minute, temperature is 100.9°F, and pulse oxygenation is 94% on room air. On examination, auscultation of the lungs reveals bibasilar crackles. Laboratory results reveal WBC 14,500/μL, hematocrit 39%, platelets 250/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 18 mEq/L, BUN 27 mg/dL, creatinine 1.5 mg/dL, and glucose 85 mg/dL. Serum lactate is 4.7 mmol/dL. Chest radiography reveals bilateral lower lobe infiltrates. Based on this patient’s presentation, which of the following is the most likely diagnosis?
Hospital-acquired pneumonia (HAP)
Community-acquired pneumonia (CAP)
Health care–associated pneumonia (HCAP)
Ventilator-associated pneumonia (VAP)
Atypical pneumonia
173. A 55-year-old man presents to the ED with fever, drooling, trismus, and a swollen neck. He reports a foul taste in his mouth caused by a tooth extraction 2 days ago. On physical examination, the patient appears anxious. He has bilateral submandibular swelling and elevation and protrusion of the tongue. He appears “bull-necked” with tense and markedly tender edema and brawny induration of the upper neck, and he is tender over the lower second and third molars. There is no cervical lymphadenopathy. These lungs are clear to auscultation with good air movement. His vital signs are HR 105 beats per minute, BP 140/85 mm Hg, RR 26 breaths per minute, and temperature 102°F. Which of the following is the most appropriate next step in management?
Obtain a sample for culture, administer a dose of IV antibiotics, and obtain a soft tissue radiograph of the neck.
Obtain a sample for culture, perform a broad incision and drainage at bedside, and administer a dose of IV antibiotics.
Administer a dose of IV antibiotics and obtain a CT scan of the soft tissues of the neck.
Administer a dose of IV antibiotics, obtain a CT scan of the soft tissues of the neck, and obtain an emergent ENT consult.
Secure his airway, administer a dose of IV antibiotics, and obtain an emergent ENT (ear, nose, and throat) consult
174. A 67-year-old woman with a history of steroid-dependent COPD, non–insulin-dependent diabetes, and hypertension presents to the ED with complaints of a painful, red, swollen left lower leg. She states she noted a “bug bite” in that area 1 week ago and since then has had gradually increasing symptoms. On examination, you note a 12 cm × 10 cm sharply demarcated area of blanching erythema, warmth, and tenderness on the medial thigh with ascending erythema to the groin. You also note tender adenopathy in the left inguinal region. Her BP is 90/55 mm Hg, RR is 24 breaths per minute, HR is 105 beats per minute, temperature is 102.4°F, and pulse oxygenation is 98% on room air. Laboratory results reveal WBC 19,500/μL, hematocrit 39%, platelets 175/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 14 mEq/L, BUN 32 mg/dL, creatinine 1.7 mg/dL, and glucose 455 mg/dL. Serum lactate is 4.7 mmol/dL. Which of the following best describes her clinical state?
She has systemic inflammatory response syndrome (SIRS).
She has sepsis
She has severe sepsis.
She is in septic shock
She has multiple organ dysfunction syndrome (MODS).
175. An 84-year-old man presents to the ED with his family due to concerns that his condition is worsening despite being placed on levofloxacin for a urinary tract infection 5 days ago by his primary care physician. His is obtunded and unable to give any additional history. Physical examination does not reveal the source of infection. His BP is 84/45 mm Hg, HR is 135 beats per minute, temperature is 102.8°F, and his RR is 28 breaths per minute. Laboratory results reveal WBC 24,500/μL, hematocrit 19%, platelets 90/μL, sodium 132 mEq/L, potassium 7.5 mEq/L, chloride 100 mEq/L, bicarbonate 12 mEq/L, BUN 37 mg/dL, creatinine 6.5 mg/dL, and glucose 255 mg/dL. Serum lactate is 11.3 mmol/dL. Cardiac enzymes and troponin are mildly elevated, and he has hyperacute T-waves on electrocardiogram (ECG). His chest radiograph shows cardiomegaly with bilateral patchy opacities and pulmonary vascular congestion. Rapid urinalysis reveals 3+ WBCs and blood and nitrates. You secure his airway with intubation, initiate broad-spectrum antibiotics, IV fluids, and other supportive therapies, and emergently consult nephrology, cardiology, and pulmonology. Which of the following best describes his clinical state?
He has SIRS
He has sepsis.
He has severe sepsis
He is in septic shock.
He has MODS
176. A 37-year-old man presents to the ED with complaints of 2 days of a sore throat and subjective fever at home. He denies cough or vomiting. His BP is 130/75 mm Hg, HR is 85 beats per minute, temperature is 101°F, and his RR is 14 breaths per minute. He has diffuse tonsillar swelling and bilateral exudates with bilaterally enlarged and tender lymph nodes of the neck. Which of the following is the next best step in management?
Administer penicillin and discharge the patient without further testing
Perform a rapid antigen test. If it is negative, confirm with a throat culture, and administer penicillin if the results are positive.
Perform a rapid antigen test. If it is negative, administer penicillin and discharge the patient.
Perform a rapid antigen test. If it is positive, administer penicillin and discharge the patient.
Discharge the patient without treatment or further testing.
177. A 37-year-old man who just finished a full course of penicillin for pharyngitis presents to the ED requesting to be checked out again. He states he took the antibiotics exactly as prescribed and initially felt somewhat improved, but over the last 2 to 3 days has had increased pain and progressive difficulty swallowing. His BP is 130/65 mm Hg, HR is 95 beats per minute, temperature is 100.1°F, RR is 16 breaths per minute, and oxygen saturation is 99%. On examination, the patient is in no acute distress but has a fluctuant mass on the right side of his neck. You visualize a normal soft palate with swelling of the right tonsillar arch and deviation of the uvula to the left, but additional examination is limited because he is unable to open his mouth fully. Review of his records reveals a throat culture that was positive for Streptococcus. Which of the following is the most appropriate next step in management?
Attempt needle aspiration, treat him with a new course of antibiotics (either penicillin or clindamycin), and have him return in 24 hours.
Give him morphine for pain control, give him a dose of IV antibiotics, and observe him in the ED for 6 hours.
Admit him for incision and drainage in the OR under general anesthesia.
Switch his antibiotic to clindamycin and have him return in 24 hours.
Order a CT scan to visualize his neck, continue the penicillin, and have him return in 24 hours
178. A 50-year-old man presents to the ED complaining of fever, headache, and neck pain for 24 hours. He states that 1 week ago he had rhinorrhea, nasal congestion, a sore throat, and occasional dry cough. He noted generalized weakness, myalgias, and malaise yesterday afternoon, and woke up today “feeling terrible.” His BP is 145/75 mm Hg, HR is 102 beats per minute, temperature is 101.2°F, and his RR is 16 breaths per minute. On examination, he is awake, alert, and nontoxic appearing although he has discomfort in his neck with flexion. He has a nonfocal neurologic examination without increased deep tendon reflexes or opthalmoplegia. There are no rashes. Which of the following CSF results is most consistent with your clinical diagnosis of viral meningitis?
Identification of viral particles on Gram stain with an elevated CSF-to-serum glucose level
A mildly elevated total protein level with a decreased glucose level
A mildly elevated total protein level with a WBC count of fewer than 500 cells/mm 3
Increased turbidity with marked xanthochromia
A markedly elevated lymphocyte count, often exceeding 100,000 cells/mm 3 with a mildly elevated total protein level
179. A 32-year-old woman presents to the ED with 7 days of vaginal discharge and pelvic pain. She is sexually active and admits to several recent “one night stands.” She denies trauma/injury and does not have any urinary or other abdominal complaints. Her HR is 85 beats per minute, BP is 135/90 mm Hg, RR is 18 breaths per minute, and temperature is 101.4°F. On bimanual examination, you note a copious, thin, white discharge with mild diffuse adnexal tenderness with significant cervical motion tenderness. There are no rashes, skin lesions, or adenopathy. Laboratory results are notable for a WBC of 18,000/μL. A urinalysis shows WBCs but is otherwise within normal limits. Which of the following is the most appropriate next step in management?
Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow-up within 1 week.
Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week.
Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better.
Give her a one-time dose azithromycin (1 g PO), and ceftriaxone (250 mg IM) with urgent gynecology follow-up within 1 week.
Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week.
180. A 45-year-old woman presents to the ED complaining of 3 days of fever and worsening throat pain and painful odynophagia without cough or coryza. She sits on a chair, leaning forward with her mouth slightly open. She is refusing to swallow and has a cup of saliva and a box of facial tissues at her side. Vitals are HR of 120 beats per minute, BP of 110/70 mm Hg, RR of 22 breaths per minute, oxygen saturation of 99% on room air, and temperature of 102.8°F. You note a slight wheezing noise coming from her anterior neck. Her voice is hoarse and she is able to open her mouth fully, making her examination quite difficult. From what you can visualize, her posterior oropharynx is moderately hyperemic, without exudates or tonsillar enlargement. A soft tissue lateral cervical radiograph shows marked edema of the prevertebral soft tissues and absence of the vallecular space. Which of the following is the most likely diagnosis?
Retropharyngeal abscess
Peritonsillar abscess
Epiglottitis
Pharyngitis
Laryngotracheitis
181. A 19-year-old woman presents with 4 days of bilateral lower abdominal pain right greater than left. She also complains of a fever, nausea, vomiting, and general malaise. Her last menstrual period was 5 days ago. Vitals are HR 98 beats per minute, BP 110/65 mm Hg, RR 18 breaths per minute, and temperature of 102.7°F. Pelvic examination demonstrates exquisite cervical motion tenderness and right adnexal tenderness. Laboratory reports are notable for a WBC 15,000/μL, an ESR of 95 mm/h, and a negative urine β-human chorionic gonadotropin (β-hCG). Transvaginal ultrasound demonstrates a right complex mass with cystic and solid components. Which of the following is the most appropriate next step in management?
Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow-up within 1 week.
Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week.
Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better.
Given her a one-time dose with emergent gynecology consultation for possible laparoscopic drainage
Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week.
182. A 42-year-old IV drug user presents to the ED with fever, chills, pleuritic chest pain, myalgias, and general malaise. The patient’s vitals include an HR of 110 beats per minute, BP of 110/65 mm Hg, RR of 18 breaths per minute, and temperature of 103.4°F. Physical examination is notable for retinal hemorrhages, petechiae on the conjunctivae and mucous membranes, a faint systolic ejection murmur, and splenomegaly. Which of the following is the most likely diagnosis?
Disseminated gonorrhea
Myocarditis
Pericarditis
Infectious mononucleosis
Endocarditis
183. A 51-year-old diabetic man complains of intense right-ear pain and discharge. On physical examination, his BP is 145/65 mm Hg, HR 91 beats per minute, and temperature 101°F. He withdraws when you retract the pinna of his ear. The external auditory canal is erythematous, edematous, and contains what looks like friable granulation tissue in the external auditory canal. The tympanic membrane is partially obstructed but appears to be erythematous, as well. You make the presumptive diagnosis of necrotizing (malignant) otitis externa. Which of the following statements regarding this condition is true?
It is an uncommon complication of otitis media in otherwise healthy patients.
The mainstay of treatment is outpatient with oral antibiotics.
Cranial nerve IX palsy is the most common complication.
Pseudomonas aeruginosa is the most common causative organism.
Hearing loss is the most common complication
184. A 26-year-old woman presents to the ED with fever, malaise, and an evolving rash in the right axilla that she initially thought was from an insect bite that she received while hiking 1 week earlier. She complains of generalized fatigue, nausea, headache, and joint pain over the past several days. Her vitals are BP of 120/75 mm Hg, HR of 75 beats per minute, RR of 16 breaths per minute, and temperature of 101°F. On physical examination, she is awake and alert, with a nonfocal neurologic examination. Her neck is supple, but she is diffusely tender over the shoulder, knee, and hip joints bilaterally without any distinct effusions. Her abdomen is soft and nontender. She has a 9-cm erythematous annular plaque with partial central clearing and a bright red outer border and a target center under her right axilla. Which of the following is the next best step?
Treat empirically with broad-spectrum antibiotics and consult dermatology emergently for a biopsy of the rash.
Treat empirically for a cellulitis with cephalexin for 10 days and arrange follow-up with her primary care doctor.
Treat empirically for Lyme disease with doxycycline for 21 days and arrange follow-up with her primary-care doctor
Treat empirically for an allergic dermatitis with prednisone, diphenhydramine, and famotidine for 3 days, and arrange follow-up with her primary care doctor.
Perform serologic testing for Borrelia burgdorferi to confirm the diagnosis of Lyme disease and arrange follow-up with her primary care doctor.
185. A 22-year-old man without medical complaints presents to the ED with a 3-day history of fever, malaise, and myalgias. He denies chest pain, shortness of breath, nausea or vomiting, abdominal pain, cough, sore throat, genitourinary symptoms, or respiratory tract complaints. On examination, the patient’s BP is 100/60 mm Hg, HR is 110 beats per minute, RR is 20 breaths per minute, and temperature is 102°F. He appears awake, alert, and comfortable. His physical examination is normal. Which of the following is the most appropriate next step in management?
Discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination
Order a CBC, urinalysis, and chest x-ray. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
Order a CBC, urinalysis, chest x-ray, and two sets of blood cultures. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. Start empiric IV antibiotics and admit him for observation.
186. A 54-year-old man with a history of hepatitis C, alcohol abuse, and cirrhotic ascites presents with increasing abdominal girth and abdominal pain. He complains of increasing difficulty breathing, especially when lying down, caused by worsening ascites. On physical examination, the patient is cachectic and appears older than his stated age. He has a diffusely tender abdomen and tense ascites. The liver is palpable 4 cm below the costal margin. Vitals include a BP of 110/65 mm Hg, HR of 110 beats per minute, RR of 22 breaths per minute, and temperature of 102°F. Which of the following is the most common organism seen in spontaneous bacterial peritonitis?
Pseudomonas aeruginosa
Enterococcus
Streptococcus pneumoniae
Enterobacteriaceae
Streptococcus viridans
187. A 30-year-old man with type 1 diabetes presents to the emergency department (ED). His blood pressure (BP) is 100/70 mm Hg and heart rate (HR) is 140 beats per minute. His blood glucose is 750 mg/dL, potassium level is 5.9 mEq/L, bicarbonate is 5 mEq/L, and arterial pH 7.1. His urine is positive for ketones. Which of the following is the best initial therapy for this patient?
A. Give normal saline as a 2-L bolus; then administer 20 units of regular insulin subcutaneously.
B. Bolus 2 ampules of bicarbonate and administer 10 units of insulin intravenously.
C. Give him 5 mg of metoprolol to slow down his heart, start intravenous (IV) hydration, and then give 10 units of regular insulin intravenously.
D. Give normal saline in 2 L bolus and then administer 10 units of insulin intravenously followed by an insulin drip and continued hydration.
E. Give normal saline in 2 L bolus with 20 mEq/L potassium chloride (KCl) in each bag.
188. A 39-year-old woman, brought into the ED by her family, states that she has had 4 days of diarrhea and has now started acting “crazy” with mood swings and confusion. The family states that she usually takes a medication for a problem with her neck. Her BP is 130/45 mm Hg, HR is 140 beats per minute, temperature is 101.5°F, and her respiratory rate (RR) is 22 breaths per minute. An electrocardiogram (ECG) reveals atrial fibrillation with a normal QRS complex. After you address the airway, breathing, and circulation (ABCs), which of the following is the most appropriate next step in management?
Administer 2 ampules of bicarbonate to treat for tricyclic antidepressant overdose.
Administer chlordiazepoxide, thiamine, and folate
Administer ceftriaxone and prepare for a lumbar puncture.
Administer propranolol and propylthiouracil (PTU); then wait an hour to give Lugol iodine solution.
Administer ciprofloxacin and give a 2-L bolus of normal saline for treatment of dehydration secondary to infectious diarrhea.
189. A 65-year-old woman, brought into the ED by her family, states that she has been weak, lethargic, and saying “crazy things” over the last 2 days. Her family also states that her medical history is significant only for a disease of her thyroid. Her BP is 120/90 mm Hg, HR is 51 beats per minute, temperature is 94°F rectally, and RR is 12 breaths per minute. On examination, the patient is overweight, her skin is dry, and you notice periorbital nonpitting edema. On neurologic examination, the patient does not respond to stimulation. Which of the following is the most likely diagnosis?
Apathetic thyrotoxicosis
Myxedema coma
Graves disease
Acute stroke
Schizophrenia
190. A 74-year-old woman who is a known diabetic is brought to the ED by emergency medical service (EMS) with altered mental status. The home health aide states that the patient ran out of her medications 4 days ago. Her BP is 130/85 mm Hg, HR is 110 beats per minute, temperature is 99.8°F, and RR is 18 breaths per minute. On examination, she cannot follow commands but responds to stimuli. Laboratory results reveal white blood cell (WBC) count of 14,000/L, hematocrit 49%, platelets 325/L, sodium 128 mEq/L, potassium 3.0 mEq/L, chloride 95 mEq/L, bicarbonate 22 mEq/L, blood urea nitrogen (BUN) 40 mg/dL, creatinine 1.8 mg/dL, and glucose 850 mg/dL. Urinalysis shows 3+ glucose, 1+ protein, and no blood or ketones. After addressing the ABCs, which of the following is the most appropriate next step in management?
Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulin intravenously
Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulin intravenously and begin phenytoin for seizure prophylaxis.
Administer 10 units of regular insulin intravenously; then begin fluid resuscitation with a 2- to 3-L bolus of normal saline.
Order a computed tomographic (CT) scan of the brain; if negative for acute stroke, begin fluid resuscitation with a 2- to 3-L bolus of normal saline.
Arrange for urgent hemodialysis
191. A 21-year-old man presents to the ED. He has a known history of type 1 diabetes. He is hypotensive with BP of 95/65 mm Hg, tachycardic at 120 beats per minute, and tachypneic at 30 breaths per minute. Laboratory results reveal a WBC 20,000/μL, hematocrit 45%, platelets 225/μL, sodium 131 mEq/L, potassium 5.3 mEq/L, chloride 95 mEq/L, bicarbonate 5 mEq/L, BUN 20 mg/dL, creatinine 0.9 mg/dL, and glucose 425 mg/dL. Arterial blood gas reveals a pH of 7.2. Urinalysis reveals glucosuria and ketosis. There is a fruity odor to his breath. Which of the following provides the strongest evidence for the diagnosis?
Hypotension, tachycardia, and tachypnea
Glucose of 425 mg/dL, ketosis, and leukocytosis
Glucose of 425 mg/dL, ketosis, pH 7.2, and bicarbonate of 5 mEq/L
Glucose of 425 mg/dL, hypotension, and fruity odor to breath
Glucosuria, hypotension, and leukocytosis
192. A 32-year-old man is brought to the ED by EMS for confusion. EMS reports that the patient was at a local pharmacy filing his prescriptions when the pharmacist noticed the patient sweating and having difficulty answering questions. In the ED, the patient’s BP is 130/68 mm Hg, HR is 120 beats per minute, temperature is 98.9°F, and RR is 12 breaths per minute. The patient is unable to explain what happened. His fingerstick glucose is 410 mg/dL and his urine is positive for ketones. An electrolyte panel reveals Na + 131 mEq/L, K + 4 mEq/L, Cl − 91 mEq/L, and Ca 2+ 11 mEq/L. Which of the following electrolytes are most important to supplement during the management of his medical condition?
Sodium, potassium, and calcium
Sodium
Potassium
Calcium
Sodium and calcium
193. A 36-year-old immigrant woman is brought to the ED from her workplace. She was found to be agitated and behaving bizarrely. The patient’s past medical history and medications are unknown. Her BP is 162/92 mm Hg, HR is 140 beats per minute, temperature is 101.8°F, and RR is 18 breaths per minute. On examination, the patient is delirious, tremulous, and has a large goiter. Which of the following is the most appropriate management of this patient?
Administer dantrolene
Administer acetaminophen and broad-coverage antibiotics.
Protect airway; administer iodine.
Administer diazepam.
Protect airway; administer acetaminophen, propranolol, and PTU
194. A 75-year-old woman is brought to the ED by EMS after she had a witnessed seizure on the street. A bystander reports that the patient fell to the ground, had tonic-clonic activity, and was drooling. Her BP is 162/85mm Hg, HR is 95 beats per minute, temperature is 99.4°F, and RR is 16 breaths per minute. On examination, the patient is unresponsive and has a bleeding superficial scalp laceration. Which of the following electrolyte disturbances is least likely to cause a seizure?
Hypoglycemia
Hyperglycemia
Hyponatremia
Hypernatremia
Hypokalemia
195. A 53-year-old woman is brought to the ED by her husband. He states that his wife is feeling very weak over the last 2 days, is nauseated, and vomiting at least three times. The husband states that she was taking a high-dose medication for her joint pain but ran out of her pills last week. Her vital signs are BP of 90/50 mm Hg, HR 87 beats per minute, RR 16 breaths per minute, and temperature 98.1°F. You place her on the monitor, begin IV fluids, and send her blood to the laboratory. Thirty minutes later the metabolic panel results are back and reveal the following: Na+ 126 mEq/L K+ 5 mEq/L Cl− 99 mEq/L HCO3 21 mEq/L BUN 24 mg/dL Creatinine 1.6 mg/dL Glucose 69 mg/dL Ca+ 11 mEq/L What is the most likely diagnosis?
Myxedema coma
Thyroid storm
Hyperaldosteronism
Adrenal insufficiency
Diabetic ketoacidosis (DKA)
196. A 44-year-old agitated woman is brought to the ED by her husband. He states that she has had fevers to 101°F and a productive cough at home for the last 3 days. Today she became labile, agitated, and complained of abdominal pain. She was recently diagnosed with Graves disease and started on PTU. Her BP is 156/87 mm Hg, HR is 145 beats per minute, temperature is 102.4°F, and RR is 20 breaths per minute. On examination, the patient is agitated, confused, and has rales on auscultation bilaterally. Which of the following is the most likely diagnosis?
Pheochromocytoma
Cocaine ingestion
Heat stroke
Thyroid storm
Neuroleptic malignant syndrome
197. An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
Sentinel loop of bowel
No gas in the rectum
Presence of an ileus
Pneumatosis intestinalis
Air fluid levels
198. A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardic with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
Parasites
Viruses
Enterotoxin-producing bacteria
Anaerobic bacteria
Invasive bacteria
199. A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/μL Sodium 131 mEq/L Hematocrit 48% Potassium 3.5 mEq/L Platelets 210/μL Chloride 101 mEq/L Aspartate transaminase (AST) 85 U/L Bicarbonate 10 mEq/L Alanine transaminase (ALT) 60 U/L Blood urea nitrogen (BUN) 9 mg/dL Alkaline phosphatase 75 U/L Creatinine 0.5 mg/dL Total bilirubin 0.5 mg/dL Glucose 190 mg/dL Lipase 40 IU Nitroprusside test weakly positive for ketones Which of the following is the mainstay of therapy for patients with this condition?
Normal saline (NS) solution
Half normal saline (1/2 NS)
Glucose solution (D5W)
Solution containing both saline and glucose (D5/NS or D5 1/2 NS)
The type of solution is irrelevant
200. As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
Plain film radiograph
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Radioisotope cholescintigraphy (HIDA scan)
Ultrasonography
{"name":"Med 1-200 .", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge and understanding of cardiovascular health with our comprehensive quiz designed for medical professionals, students, and enthusiasts alike. Featuring 200 challenging questions, this quiz will help you assess your expertise in diagnosing and managing heart-related conditions.Key Features:200 questions covering a range of cardiovascular topics.Multiple-choice format to test critical thinking and decision-making skills.Ideal for studying for exams or enhancing your medical knowledge.","img":"https:/images/course8.png"}
More Quizzes
IM paraclinique new* HKS
117580
(NEW)part8(1957-2000)......(1785-2039)6breetpit
108540
What character from "The Quiltmaker's Gift" are you ?
8419
Computer Vision
1050
Free Excel Certification Practice Test
201027078
Can You Master These Funny Chemistry Test Answers?
201032385
Anatomy Tissue: Identify Tissues & Their Locations
201032385
Dog Island: Challenge Yourself with Buffalo Trivia!
201041778
Unlock Your Energetic Signature: Take the Free
201033233
Number the Stars Chapter 7 & 8 Challenge
201068817
Master Scatter Plot Questions: Free Correlation
201027626
Introduction to Data Analytics
15819872