Chapter 8 Skin Disorders Test: What Is a Papule?
Quick, free papule quiz to test your knowledge. Instant results.

This quiz helps you spot papules and other primary lesions from Milady Chapter 8, so you can check your understanding fast. For extra practice, try the manual comedone removal quiz, explore dermatology quiz questions, or build ID skills with a skin disease quiz.
Study Outcomes
- Identify Milia Characteristics -
Describe the defining features of milia and recognize their presentation on various skin types.
- Classify Skin Lesions -
Differentiate between primary and secondary lesions, such as macules, papules, and pustules, for accurate diagnosis.
- Distinguish Skin Discolorations -
Understand terminology for brown or wine-colored discolorations and apply the correct diagnostic labels.
- Recognize Dermal Fissures -
Identify cracks in the skin that penetrate the dermis and associate them with appropriate treatment considerations.
- Apply Dermatological Terminology -
Use proper clinical terms for various skin disorders and diseases to enhance communication accuracy.
- Evaluate Exam Readiness -
Test your knowledge through scored quiz questions to bolster confidence and prepare for cosmetology exams.
Cheat Sheet
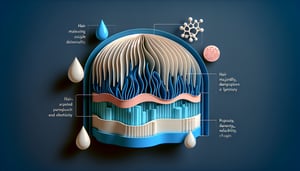
- Understanding Primary and Secondary Lesions -
Primary lesions appear on previously unaltered skin - common examples include papules, vesicles, and pustules - while secondary lesions, such as crusts, scales, and scars, arise from the evolution or external manipulation of primary lesions. A simple mnemonic is "Primary Pops, Secondary Sequel" to track lesion progression. This classification is essential for the Milady Chapter 8 Test on skin disorders and diseases, ensuring you differentiate lesions confidently (Source: American Academy of Dermatology).
- Characteristics of Milia -
Milia are tiny, 1 - 2 mm white keratin-filled cysts that often dot the cheeks and under the eyes, appearing as "milk spots" in newborns and adults alike. They stem from trapped keratin under the skin's surface and require gentle exfoliation or professional extraction. The phrase "Milia Milk" can help you recall their signature appearance and benign nature (Source: NIH Dermatology Library).
- Flat Discolorations - Macules vs. Patches -
Flat lesions are called macules if they're under 1 cm (like freckles) and patches if they're larger (such as port-wine stains). Despite varying colors - from brown to wine-red - their classification hinges solely on size and flatness, not hue. This rule, emphasized by dermatology texts at Johns Hopkins, is a must-know for the Milady Chapter 8 test.
- Identifying Fissures -
Fissures are linear cracks extending into the dermis, commonly seen in conditions like angular cheilitis or athlete's foot, and they often bleed or sting. Keeping skin hydrated with emollients and applying barrier creams can prevent infection and promote healing. The Mayo Clinic highlights proper moisturization as key to managing these painful breaks.
- Pigmentary Disorders: Melasma (Chloasma) -
Melasma, often dubbed the "mask of pregnancy," manifests as brownish patches on sun-exposed areas and is triggered by UV radiation and hormonal changes. A quick mnemonic - "MELASMA = Mothers Exposed to Light And Solar Melanin Amplified" - can help you remember its etiology. The American Society for Dermatologic Surgery notes that strict sun protection is crucial for both prevention and treatment.